After meeting a leukemia survivor at an event organized on November 25 by the Capucine Foundation to raise funds, Why Doctor takes stock of this cancer which affects around 9,000 people each year in France.

Leukemias include several types of blood cancers, and affect approximately 9,000 people each year in France. If the survival rate is rather positive (more than 80% of children with acute lymphoblastic leukemia recover definitively, and less than 20% relapse), in adults, on the other hand, the results are darker. The treatments are heavier, have side effects and frequent relapses. After meeting a leukemia survivor at a November 25 event organized by the Nasturtium Foundation to raise funds to fight this disease, Why Doctor takes stock of the situation.
Leukemia, what is it?
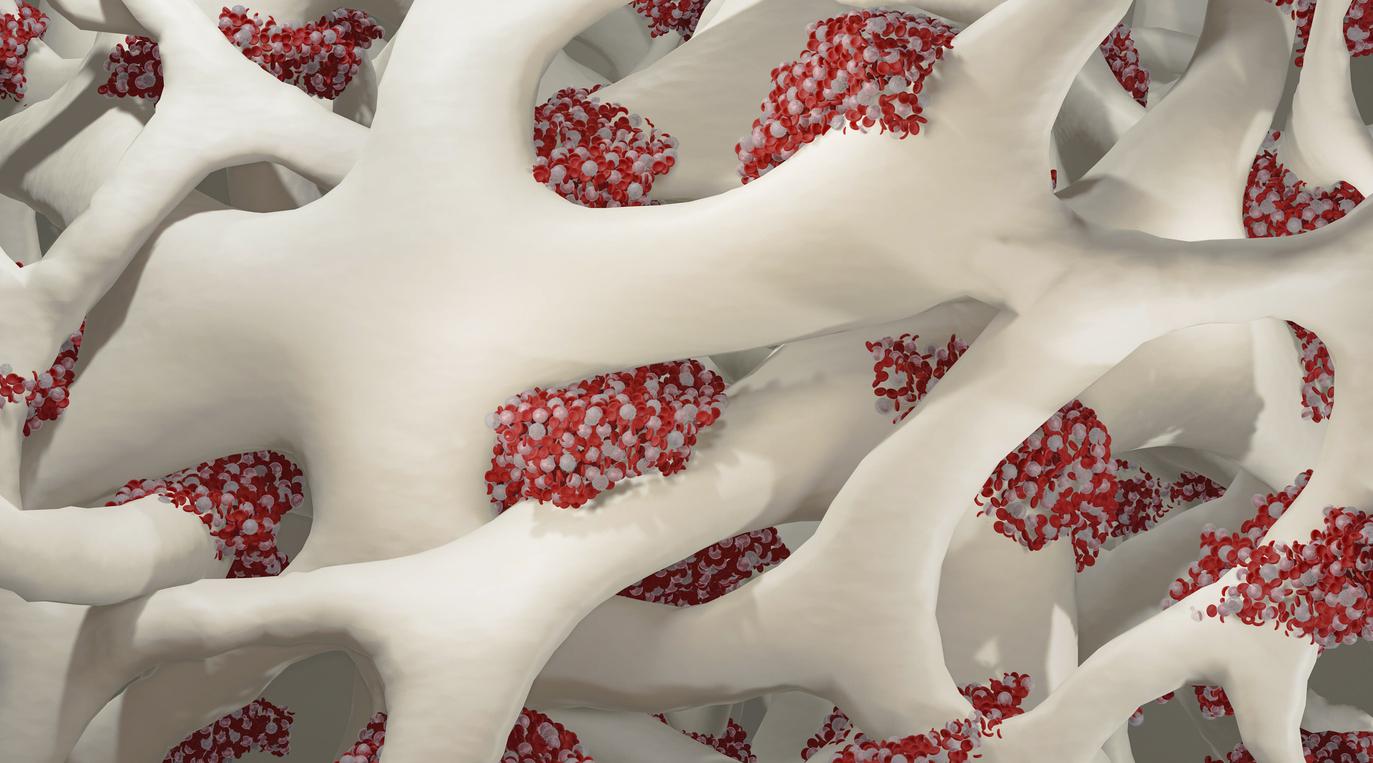
Leukemia is a form of blood cancer manifested by the proliferation of young cells in the bone marrow and blood. These are most often immature cells which, instead of maturing and ensuring the transport of oxygen, coagulation and the defense of our organism against microbes, remain blocked and invade the bone marrow, preventing it from create normal, functional blood cells.
There are several forms of leukaemia. Depending on the degree of maturity of the abnormal cells, and the molecular abnormalities, the disease is said to be myeloid or lymphoid.
Finally, leukemia, myeloid or lymphoid, can be acute or chronic. The first evolves very quickly: the leukemic cells invade all the bone marrow, the blood, then most of the organs. If left untreated, it is rapidly fatal. In the case of chronic leukemia, the malignant cells are generally well differentiated and the symptoms appear later, less noisily.
Who is affected?
For chronic forms, in 2013, Public Health France estimated the number of people affected at around 5,200, with a greater predominance of the chronic lymphoid type (4,460 estimated cases). In detail, it mainly affects seniors and especially men: it represents 40% of leukemias in subjects over 65 years old. Given the age of the patients, most often they do not die of their hematological disease. The chronic myeloid leukemia (CML) East as for it much rarer since it concerns 15 to 20% of leukemias of the adult.
As for acute leukemia, more than 3,250 new cases were diagnosed in France in 2012, ie 1% of all cancers. Acute myeloid leukemia (AML) is the most common in adults. Its frequency increases with age. Acute lymphoblastic leukemia (ALL) is the most common acute leukemia in children. It occurs mainly between the ages of 2 and 15 and is rare in adults.
Apart from very rare cases of chemical and radiological origin, the causes of this cancer are still poorly understood.
How do we know we are sick?
At the start of the disease, the patient will suffer from fever, repeated infections (pneumonia, bronchitis, persistent angina despite antibiotics, etc.), fatigue linked to anemia or even weight loss. Since blood clotting is painful, bruising or abnormal bleeding may also occur. Finally, patients may suffer from lymph nodes, skin and even brain damage.
When the first symptoms appear, the patient most often goes to his doctor who then prescribes a blood test. The diagnosis is made according to a blood count, the NFS, which shows a decrease or an increase in the number of white blood cells, a decrease in red blood cells and platelets, depending on the type of leukemia. A bone marrow examination (myelogram) then confirms the diagnosis and the type of leukemia by analyzing the cells of the bone marrow. The latter are taken under local anesthesia at the level of the sternum or the iliac bone. A genetic and molecular analysis of leukemic cells makes it possible to better specify the type of leukemia and its prognosis.
“I was 24 when it hit me. I was a medical student and I quickly understood what it was about as well as the urgency of my doctor to send me to the hospital. The evening of my hospitalization, I went to see my parents, I told them that I was fine and that I was going to see them for no reason. That evening, I wanted to see them but I didn’t dare tell them the truth because I was too afraid of dying. It was the worst night of my life and I thought I would never see daylight again. The diagnosis was fairly quick and they explained to me that fortunately medicine had made progress but my only hope was to have a transplant”, testifies Ian, 31 years old and survivor of leukemia during a concert organized at the New Morning (Paris 10and) by the Capucine Foundation to raise funds.
What treatments?
Once the diagnosis is established, the patient is quickly admitted to the hospital in a specialized blood disease ward, in a sterile area to avoid all infections while waiting for the normal white blood cells to reappear after treatment.
Chemotherapy is then given intravenously with the aim of destroying the young and diseased cells that are multiplying in the bone marrow and blood. You then have to wait four to six weeks for healthy cells to grow again. During this period, the patient is weakened because he has very few normal blood cells. It requires blood transfusions and is monitored several times a day in case an infection appears.
“After my diagnosis, we started the treatments, chemotherapy, radiotherapy, I lost 20 kilos of muscle. My day after that was just going from bed to chair, I couldn’t stand for too long because I was tired. If I had to take a shower, I had to think beforehand to organize myself,” says Ian.
Chemotherapy can then be combined with a bone marrow transplant, a semi-liquid spongy tissue present throughout the skeleton, part of which produces the various blood cells. The donor can be part of the family: in theory, a patient has a one in four chance of being compatible with his brother or sister, because there are four different possibilities for the distribution of antigens HLA.
When there is no compatible donor in the siblings, it is necessary to find a compatible unrelated donor. The doctor then contracts the register France bone marrow transplant to find, at national or international level, a donor whose genetic characteristics are as close as possible to those of the patient.
“I have three siblings but none were compatible to give me bone marrow so we went back to chemo and radiotherapy and one day luckily I found my donor, anonymous. He is not French but German, because fortunately, we benefit from European mutual aid, explains Ian, for whom very fortunately the story ends well. Thanks to him, I was transplanted, I was able to resume my studies and my girlfriend at the time is now my wife.”
Where is the research?
Although much progress remains to be made, new therapeutic strategies are regularly developed and improve the results. They consist of using therapeutic antibodies to specifically target leukemia cells in order to bring them closer to our immune system cells and destroy them. Moreover, small molecules have been developed to specifically inhibit proteins responsible for leukemia. We will then speak of targeted therapy.
Recently, researchers from University of Texas MD Anderson Cancer Center found that combining immunotherapy and chemotherapy might work well for people with acute myeloid leukemia. CD3 cells were particularly responsive to the drug combination. “This could be a biomarker on which to rely to choose the patients who can benefit from this combination of treatment”, explained Naval Daver, the research director, in his paper.
For research to continue to advance, funds are needed, always more funds. “You have to think positively and whatever you give will count in the balance,” concludes Professor Perbal, supported by the Capucine Foundation.

.