After eight years of diagnostic and therapeutic wandering, Émilie Schmitt learned that she suffered from pelvic congestion syndrome, often confused with endometriosis. A relief that results from a conversation with a friend, whose father is an interventional radiologist. She tells us how this exchange changed her life.

- While Émilie Schmitt, now 26 years old, suffered from chronic pelvic pain since 2013, she was diagnosed with pelvic congestion syndrome in 2021.
- His disease, during which the pelvic veins are diseased, is treated by embolization. At the same time, the cause of pelvic congestion syndrome, a malformation linked to May Thurner syndrome, is also addressed.
- The same year, the young woman and another patient created the Congestion Pelvienne France association so that “women’s health” was not “in the hands of fate and luck.”
“At the end of middle school, I got my period for the first time. At first, I had pelvic pain related to my menstrual cycle, that is, before and during my period. Gradually Over the years, they became insidious and disconnected from my cycle. I started to have pain almost all the time. In short, we went from 7 days of suffering per month to 28 days out of 31”. confides Émilie Schmitt, now 26 years old. To combat her ailments, she used painkillers, antispasmodics, such as Spasfon, and anti-inflammatories during her years in high school. “If in the first months, I managed to stay the course, from a certain moment, this was no longer the case, because the pain had taken over my life. I had the impression that as the sand, my life slipped through my fingers.”
“On the advice of doctors, I changed pills about 15 times”
Seeing that the medications were more or less effective and that the pain had a huge impact on her school and adolescent life, her mother, a general practitioner, took “instinctively” things in hand. “In 2016, three years after the first manifestations, she suggested that I consult a gynecologist. She directed the specialist to look for endometriosis.” At the end of this appointment, the young patient performs an ultrasound. “On this examination, we see a small thickening of the ligaments, but nothing could explain the pain. No solution could be found, so I continued to have pain. In addition, colic and digestive problems often appeared It was also very complicated for my sex life, because I had pain during and after intercourse. At that time, my boyfriend, for whom this situation was also difficult, became my caregiver.
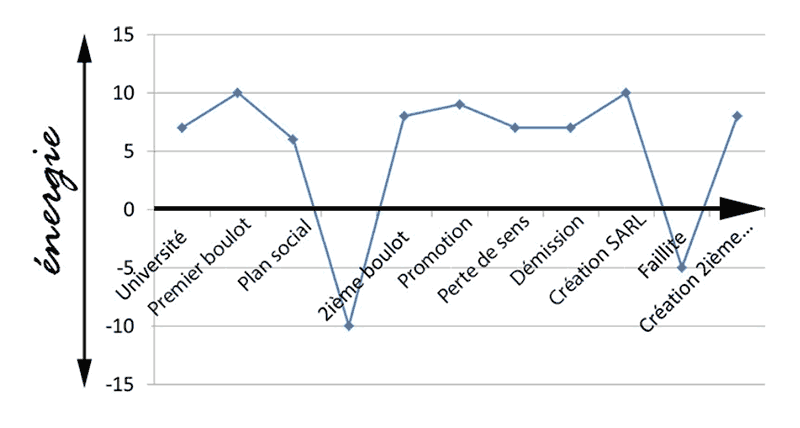
Due to her chronic suffering, her mother does not give up and motivates her. After her two years of PACES (First Common Year of Health Studies), the student managed, thanks to several requests from her mother, to benefit from a pelvic MRI. Problem: the results do not turn out to be conclusive. “Some professionals said that my pelvic pain was probably linked to my contraception. On the advice of doctors, I changed pills about 15 times. But nothing had any effect. It was a fairly dark period, even one of depression . I felt alone. I was in redemption and acceptance, I told myself that my life was going to be like this forever. I turned to self-hypnosis and sophrology. of the stronger and stronger treatments, like Tramadol Since this medication was getting me high, I couldn’t study and I ended up doing retakes all the time. At times, I really wondered if it was really worth continuing. to live”, remembers the intern in gynecology and obstetrics, who is currently working in Guyana. Fortunately, the twenty-something is surrounded and supported by her “lover”his family and his friends. “They were very present and helped me fight.”
“I have varicose veins all over my stomach”, “this is potentially pelvic congestion syndrome”
One day, luck smiled on him. “After my addiction to painkillers, I told a friend at university about my suffering. I completely emptied my bag and my hatred. During the conversation, the latter replied to me that his father, an interventional radiologist, takes care of of a condition called pelvic congestion syndrome, which is similar to my symptoms. He advises me to give him my pelvic MRI in CD so that his father can study it. Fifteen days later, I receive a call from his father. Doctor Quentin Sénéchal. He tells me that I have varicose veins all over my stomach and that it is potentially a syndrome.” In order to confirm the diagnosis and quickly enter into a course of care, the practitioner asks to receive it at the Center Cardiologique du Nord in Saint-Denis
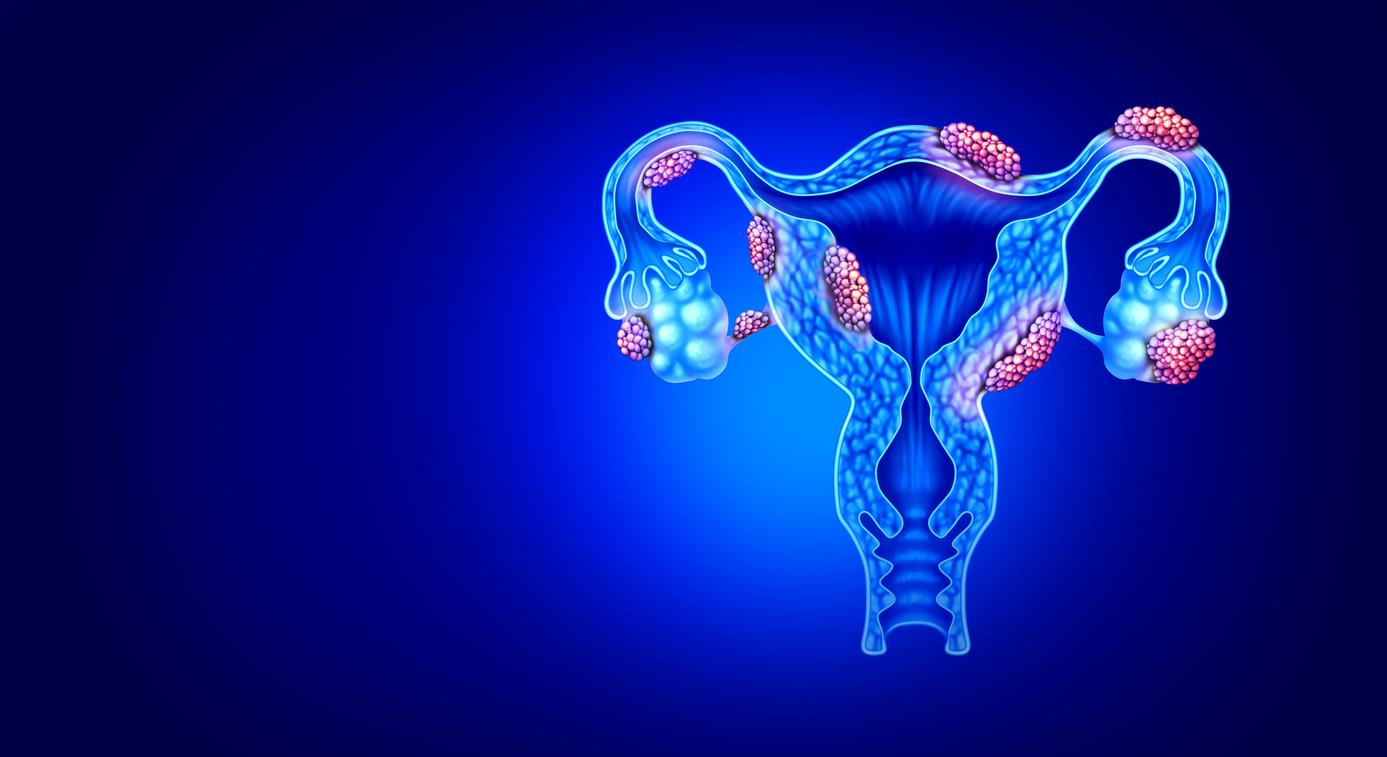
Indeed, several criteria must be checked to declare that it is pelvic congestion syndrome. “It is a disease of the vessels, which often appears after pregnancy. More precisely, it is the pelvic veins which are diseased. Among women with pelvic varicose veins, in some they are asymptomatic and in others they can cause pain When establishing the diagnosis of this pathology with gynecological, urinary and digestive expression, it is necessary to identify an association between pelvic varicose veins and the symptoms. chronic pelvic pain located in the lower abdomen or pelvis lasting more than six months, which is permanent or cyclical, pain occurring at the end of the day or aggravated by standing or sitting for a long time, hemorrhoids, diarrhea, constipation, permanent cystitis, tingling in the swollen vulva, varicose veins of the labia majora and on so-called atypical limbs, such as the thighs or buttocks, and finally post-coital pain.”
Pelvic congestion syndrome: a malformation linked to May Thurner syndrome in question
When she arrives at the clinic, the former Parisian performs a Doppler ultrasound. Then, over 15 days, an update on his symptoms is taken. Given that all the signs have been identified in the intern, the practitioner confirms that she has pelvic congestion syndrome, from which one in 20 women suffer, according to estimates from the Pelvic Congestion France associationbased on the Constances cohort, created by Émilie Schmitt and Nacira Martin three years ago. “The announcement of the diagnosis was a middle finger to all those who called me crazy, a revenge on life.” After further examinations, doctors were able to determine the cause: a malformation linked to May Thurner syndrome. “In this disease, an artery compresses and presses on the iliac vein and presses it against the spine.”
In February 2021, specialists offered pelvic embolization, the standard treatment for pelvic congestion syndrome. “I accepted, because I had no immediate desire to become pregnant.” Before the procedure, a venogram is performed. “This radiological examination allows you to see the varicose veins after the injection of an iodized contrast product. Then, during the embolization, under general or loco-regional anesthesia, the healthcare professionals block the diseased networks. After the operation , I had a lot of pain, it took me six months to recover. Subsequently, it was found that my iliac vein was no longer compressed, because the embolization favored blood reflux. It was still necessary to treat May Thurner syndrome. For this, they put a stent in my vessels.”
“No more pain” after pelvic embolization
The patient needed treatment with physiotherapy to reduce inflammation and relearn how to listen to her body, as well as psychotherapy and sexology to better understand her sexual and relationship life. “It took me two years, but all these weapons helped me get through it. Today, it’s no longer necessary to carry around with painkillers, to leave them in my friend’s car or at university, because I no longer have pain. It changed my life. Recently, I was able to hike to Machu Picchu, it’s one of the greatest gifts my body can give me after. years of suffering”, exclaims the president of the Congestion Pelvienne France association which supports patients, a reference for member doctors and trains midwives, gynecologists, general practitioners and even physiotherapists.
“The association was created because we did not want, with the members, Julie Cousin and Johanna Lalandes, that women’s health, which cannot wait, be in the hands of destiny and luck, as was the case. been for me, because unfortunately, many gynecologists do not know about congestion syndrome or do not believe that this disease exists. Those affected must know that they are not the only ones to suffer. Even in the darkest times, the. evening in bed after crying, being dispossessed by medication, we must not give in to loneliness. The pain is not in the head!”