Advances in genetics have given a tremendous boost to predictive medicine. But what credit should be given to the reliability of these tests and how to interpret them?
Being cured before you even get sick is the promise of predictive medicine. This is now experiencing a tremendous boom with, in particular, the development of new imaging technologies and the development of genetic knowledge that allow us to better understand the mechanisms of the appearance of diseases. However, most often these are techniques capable of assessing the risk of developing a disease and not of predicting its onset, which raises a number of ethical and practical questions.
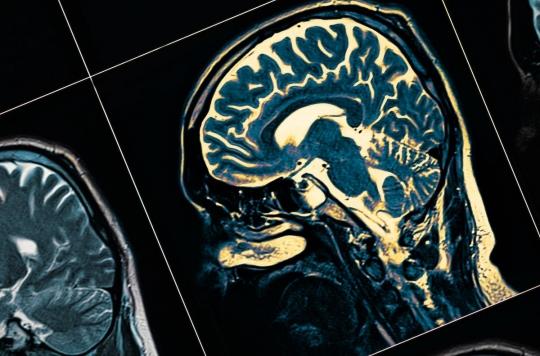
Medical imaging is now able to explore the human body in every nook and cranny. The most recent techniques make it possible, for example, to visualize neurological activity and, in certain cases, to detect elements indicative of the presence or development of a disease. It is thus possible to detect Alzheimer’s disease earlier and earlier. However, no treatment is available for this pathology, regardless of the stage at which it is detected.
This is one of the major questions raised by these new approaches: what to do with the information acquired? Ségolène Aymé, geneticist, recalls that “in predictive medicine, there is medicine. We need to ask ourselves what we can do with this new data to be of service to the patient. Today, most often, we are not there yet ”. Genetic medicine has applications, however, including the discovery of predisposing genes. The detection of a mutation in the BRCA1 gene, which induces a 50% risk of developing breast cancer before the age of 50, offers the women concerned possibilities: to increase surveillance by mammography or to opt for a total removal of the breasts which reduces then the risk to 2%. An option widely practiced in the United States with major psycho-social consequences.
Advances in human genetics have also widely opened up the field of prediction and the difficulty of interpreting data. Many websites now offer, outside our borders, a whole range of remote genetic tests that allow their customers to know their risk of developing a given pathology: cancer, diabetes, glaucoma.
Besides the fact that the vast majority of these tests have not been scientifically validated, they provide information that has no individual value. An identical genetic mutation can mean, for one person, the development of a serious illness and, for another, a complete absence of symptoms depending on their racial origin, environment, lifestyle and many other criteria. . Ségolène Aymé is categorical: “these tests are simply a scam. They have no individual predictive value and cannot lead to any therapeutic solution other than good lifestyle advice, applicable to everyone ”. This doctor, however, is not opposed to the dissemination of these tests of “recreational” value, provided that the public is clearly informed of what they really mean. Didier Sicard, honorary president of the National Consultative Ethics Committee, and who also participated in the preparation of the exhibition, is more circumspect.
“Everyone necessarily carries a ‘genetic bomb’ in their genome and it is not necessarily necessary to have all this knowledge which generates anxiety”. He also underlines the drawback that, even if it were possible to reduce the risks thus detected, it would be dangerous to always want to go towards the least risk: “we would go towards a society which, in the end, has lost all hope”.
Doctors confronted with patient concerns
The situation in France is exceptional in Europe and in the world since genetic information is protected by laws which only allow genetic testing within a restrictive legal or medical framework. The pre-implantation diagnosis, which of course poses serious questions vis-à-vis the eugenic temptation, is today limited to serious and incurable pathologies. It mainly concerns families suffering from their desire to have a child and only represents a hundred tests carried out each year in three approved centers.
Despite the ban, more and more people are practicing these tests through websites. Rich in the information thus gathered, many of them will share their concerns with the doctor. The latter must be able to provide them with a clear answer and remind them, in particular, that the concept of risk has no predictive value and that these tests only have a very relative meaning. “
In fact, the main achievement of genetic research is to have made it possible to understand that the human genome, contrary to the exaltation of the beginnings, has yet revealed only a tiny part of its secrets. Only monogenic diseases, about fifty in total and about twenty of which are already perfectly identified, benefit from advances in predictive medicine.
For clinical and therapeutic aspects, specialists rely more on the decryption of proteins resulting from the expression of the genome. Its regulation could have more targeted and therefore more effective therapeutic implications.
.