Cognitive-behavioral therapy would be effective in reducing a negative cognitive and emotional response that amplifies pain.

- Cognitive behavioral therapy is a talking therapy that aims to combat intrusive thoughts.
- In patients with fibromyalgia, it resulted in greater reductions in chronic and diffuse pain as well as pain interference and symptom impact.
- This psychotherapeutic treatment also reduced connectivity between brain regions associated with self-awareness, pain and emotion processing.
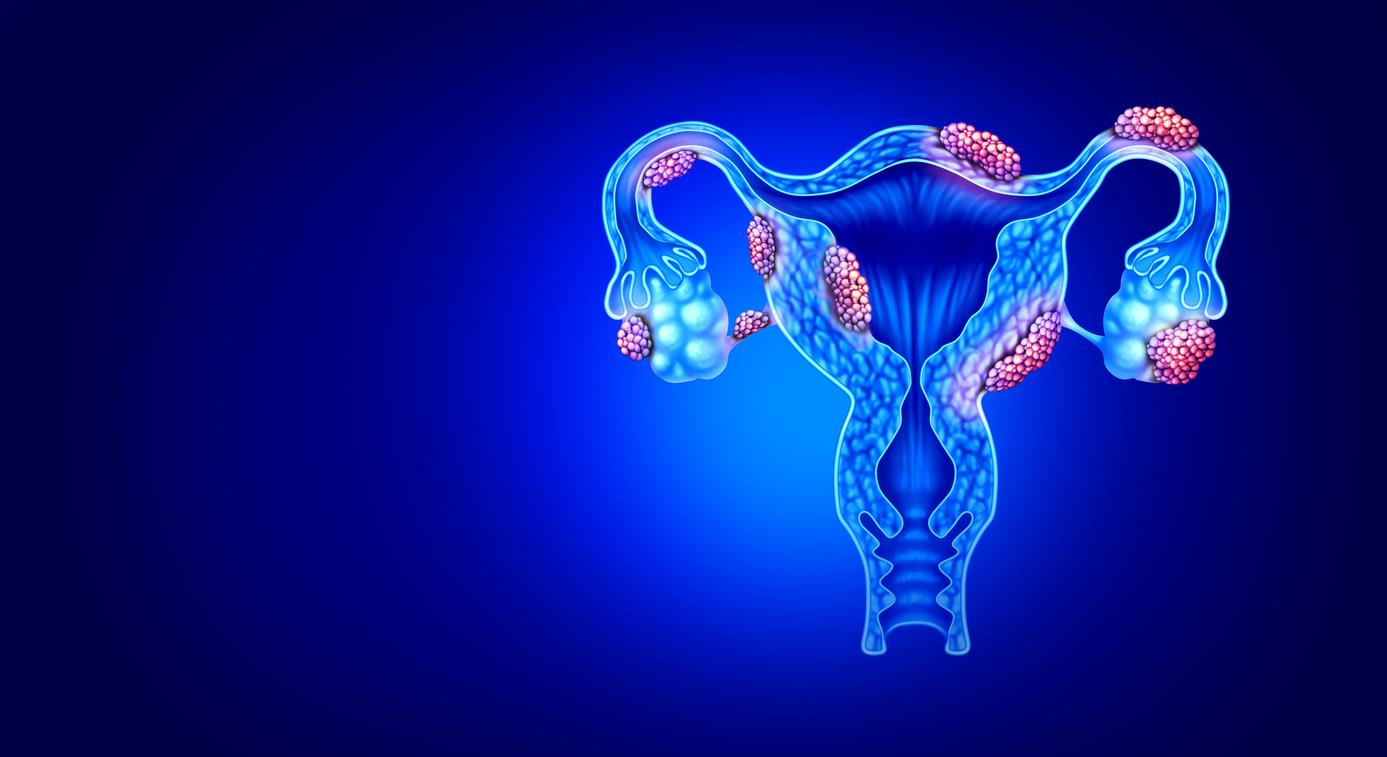
Between 1.5 to 2%. This is the proportion of the population affected by fibromyalgia in France, according to health insurance. This chronic pathology, which is more common in women, is characterized by persistent diffuse pain and sensitivity to pressure. Patients often suffer from an impaired quality of life and experience difficulty in daily activities due to the pain they experience. The diagnosis and treatment of fibromyalgia may be lacking or not appropriate, leaving many patients without satisfactory solutions to relieve their pain.
Cognitive-behavioral therapy, a promising solution for reducing pain
As part of a recent study, American researchers looked at the effectiveness of cognitive-behavioral therapy, which aims to combat intrusive thoughts, in the treatment of fibromyalgia. For the purposes of the work, they recruited 98 women, with a diagnosis of fibromyalgia confirmed for at least six months, who completed several questionnaires on pain and quality of life.
Then, 64 participants benefited from cognitive-behavioral therapy and 34 volunteers followed training on fibromyalgia and chronic pain for 8 weeks. Each intervention session included 60-75 minute consultations with a psychologist, who assessed their levels of pain interference or how pain disrupted their daily activities.
The results, published in the journal Arthritis & Rheumatology, showed that cognitive behavioral therapy led to a significant reduction in chronic and widespread pain in patients with fibromyalgia. In addition, it also reduced the interference of pain in patients’ daily activities and the impact of symptoms.

Fibromyalgia: changes in patients’ brains
The team also found that after receiving cognitive behavioral therapy, patients showed brain changes suggesting less focus on pain. “Before the participants underwent therapy, we observed that parts of the brain related to self-awareness and emotion were highly connected, suggesting that the sufferers were acutely aware of the sensation of pain they were experiencing and internalized these symptoms. After psychotherapeutic treatment, these bonds were significantly less strong, suggesting that patients were better able to detach and manage their pain after therapy. Jeungchan explained. Lee, author of the research, in a statement.