An increasingly common clinical practice, electric shock, or cardioversion, restores and maintains a regular sinus rhythm. In honor of Atrial Fibrillation Action Week, Why Doctor provides an update on this procedure.

- In the event of atrial fibrillation, an electrical cardioversion can be offered to the patient: this involves briefly passing an electrical current through his chest to resynchronize the cardiac cells and thus restore a regular heart rhythm.
- This treatment is 90% effective but requires finding the factors causing the arrhythmia to prevent recurrence.
Heart disorder affecting up to 750,000 French people, atrial fibrillation, formerly called atrial fibrillation, is characterized by an acceleration and irregular heartbeat. This irregular sinus rhythm can cause clots to form in the atrium cavity of the heart, which can then travel from the heart to the brain and cause a stroke. Atrial fibrillation can also cause the lower chamber of the heart to weaken, causing fluid buildup or heart failure.
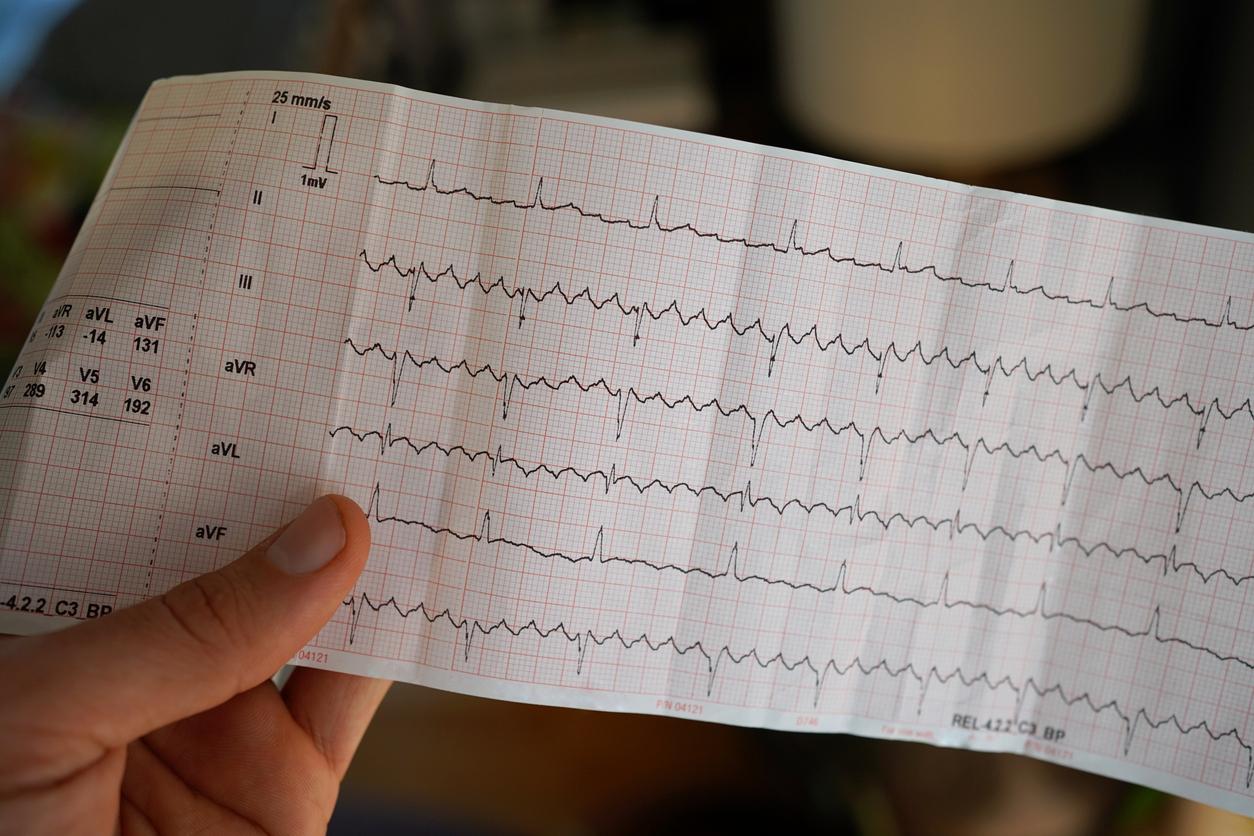
Among the treatments used for atrial fibrillation is electrical cardioversion. Unlike defibrillation, which uses more electrical energy to the chest, cardioversion uses less intense electrical shocks to resynchronize heart cells and thus restore a regular heart rhythm.
How is electrical cardioversion performed?
If complications are rare in the case of electrical cardioversion, this intervention does however require general anesthesia. It is prepared upstream with the cardiologist. “It takes between 3 weeks and a month of effective anticoagulation and an anesthesia consultation before proceeding with the electric shock, explained in December 2020 to Why Doctor Dominique Dabuty, cardiologist at the University Hospital of Tours. The interest is that very often during this less anticoagulant preparation, some of the patients will spontaneously return to a sinus rhythm.
The operation, which lasts no more than 5 minutes, takes place on an outpatient basis, on an empty stomach during a brief general anesthesia in the hospital. One or more electric shocks will be delivered to restore sinus rhythm. “When the charge is ready, we take the paddles and we deliver the electric shock by applying it to the patient’s chest. We have to make sure that the paddles take the headset in their field. By pressing like this, we deliver energy to restore a normal heart rhythm”explains Doctor Xavier Waintraub, cardiologist at La Pitié-Salpêtrière hospital in Paris.
In case of insufficient anticoagulation, cardioversion can be postponed because it exposes to a risk of intracardiac clot formation and stroke.
What are the risks and the success rate?
Electrical cardioversion makes it possible to restore 90% of a normal sinus rhythm, but this success rate can be reduced depending on various risk factors: the length of the arrhythmia, vavular damage, obesity, etc. It does not eliminate either more the cause of arrhythmia. To prevent a recurrence, antiarrhythmic treatment or ablation of atrial fibrillation can be proposed.
As for the risks, besides that of general anesthesia, cardioversion can lead to a heartbeat that is too slow or another faster arrhythmia. In case of insufficient anticoagulation, a thromboembolic accident by migration of an intracardiac blood clot can also occur.
What are the consequences of the operation?
In the absence of complications, the patient can resume a normal daily life a few days after the operation. However, he must continue his anticoagulant treatment. Its antiarrhythmic treatment can also be adapted. A point is made with the cardiologist approximately 1 month after the intervention to check the maintenance of the sinus rhythm. Two situations can then arise, lists Dominique Dabuty. “Either the cardiologist raises lifelong anticoagulation because he has so-called high-risk atrial fibrillation or we stop because the patient is better.”

Below, our Q&A program on atrial fibrillation:
.