A new clinical trial demonstrates the effectiveness of a treatment technique for atrial fibrillation: ablation by isolation of the pulmonary veins. This method reduces the symptoms of this disease and improves the quality of life of patients. A major advance in the treatment of this common heart disease.
- Pulmonary vein isolation ablation significantly reduces atrial fibrillation.
- This method also improves the quality of life of patients by reducing their symptoms.
- The SHAM-PVI study confirms that ablation is an effective and safe option for treating AF, compared with placebo.
Atrial fibrillation, often abbreviated to AF, is a very common heart condition. It is characterized by an irregular heartbeat, which can cause symptoms such as palpitations, severe fatigue, and sometimes dizziness. In addition to being uncomfortable, AF also increases the risk of stroke.
Until now, AF treatment has mainly relied on drugs called antiarrhythmics, which are designed to regulate the heartbeat. However, these drugs do not always work, or can cause unwanted side effects. That is why researchers have developed an alternative method called pulmonary vein isolation ablation, or simply ablation. This treatment involves blocking the abnormal electrical signals in the heart that cause AF by creating small, controlled lesions using a catheter.
Patients treated with ablation feel better in their daily lives
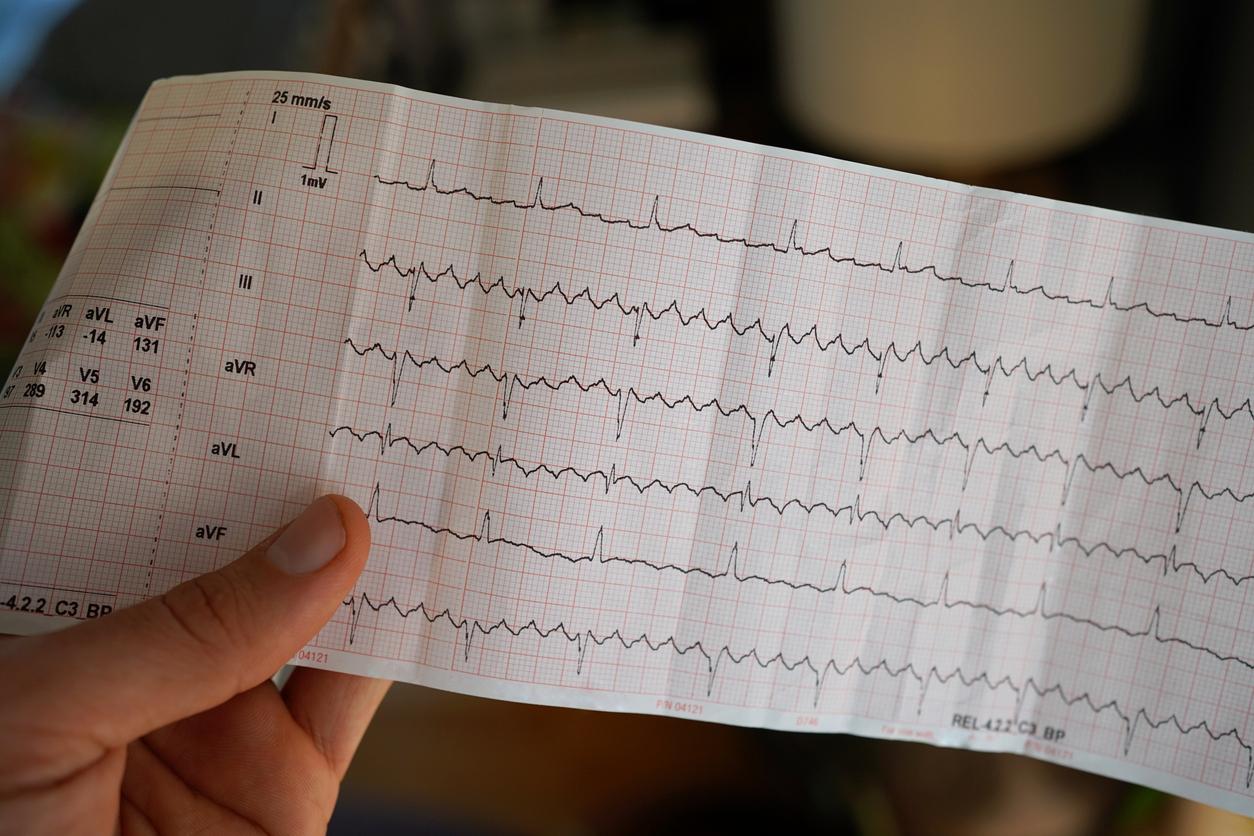
Despite the success of ablation, there was a lack of solid evidence to show its effectiveness compared to a placebo (a dummy treatment). This was sought to prove by the SHAM-PVI trial, a research project conducted in the United Kingdom, which compared real ablation with a placebo procedure. This trial involved 126 patients with AF, who were divided into two groups: 64 people received cryoablation, a technique where cold is used to treat the affected areas of the heart, while 62 underwent a placebo procedure.
The primary objective of the study was to measure the reduction in “AF burden,” that is, the percentage of time patients were in fibrillation. The results, after six months of follow-up, revealed a clear difference between the two groups. Those who received ablation saw their AF burden reduced by an average of 60%, while in the placebo group, this reduction was only 35%. For patients with persistent AF, the reduction was even greater in the ablation group, reaching 71%.
In addition to reducing the time spent in AF, the study also showed that patients treated with ablation felt better in their daily lives. They reported having fewer symptoms, being more physically active, and experiencing less anxiety related to their condition.
Treating AF in patients who do not tolerate antiarrhythmic drugs well
The SHAM-PVI trial is notable for its scientific rigor. It was conducted in a “double-blind” fashion, meaning that neither patients nor doctors knew who actually received the ablation and who received the placebo procedure. This prevents patients’ or doctors’ expectations from influencing the results. This approach therefore ensures more reliable conclusions.
The results of this trial confirm that ablation is an effective method of treating AF in patients who do not tolerate antiarrhythmic drugs well or for whom antiarrhythmic drugs no longer work. With these robust data, physicians can now refer patients with symptomatic AF to ablation with greater confidence.
Another important point highlighted by the study is the overall improvement in the quality of life of patients treated with ablation. They reported feeling better physically, but also emotionally, with less anxiety related to their disease. This is crucial, as AF can have a considerable impact on the daily lives of those who suffer from it, sometimes preventing them from leading a normal life.
Additionally, patients with persistent AF, a more severe form of the disease, particularly benefited from ablation, which may encourage more people to consider this treatment option earlier in their medical journey.
Promising prospects
These results open the way to further research. For example, it would be interesting to test this ablation method on younger patients or those with other health problems to see if it is also effective in these cases. In the long term, this technique could become a standard treatment for all people with AF, especially those who do not respond well to medication.
Additionally, the SHAM-PVI study may prompt evaluation of other types of ablation, such as radiofrequency or laser, to determine whether one of these approaches is even more effective for some patients.
How is an ablation performed to treat atrial fibrillation?
Ablation to treat atrial fibrillation is a minimally invasive procedure performed in a hospital setting. Here are the main steps:
– Patient preparation: the patient is usually sedated or given light anesthesia. A catheter is inserted into a vein, often in the groin, to access the heart.
– Heart mapping: Using real-time imaging, the doctor identifies the areas of the pulmonary veins where the abnormal electrical circuits responsible for the fibrillation are located.
– Ablation: Using heat (radiofrequency) or cold (cryoablation), small lesions are created on the heart tissue to block these abnormal electrical signals.
– End of the intervention: the catheter is removed and the patient remains under surveillance to check the effectiveness of the intervention.