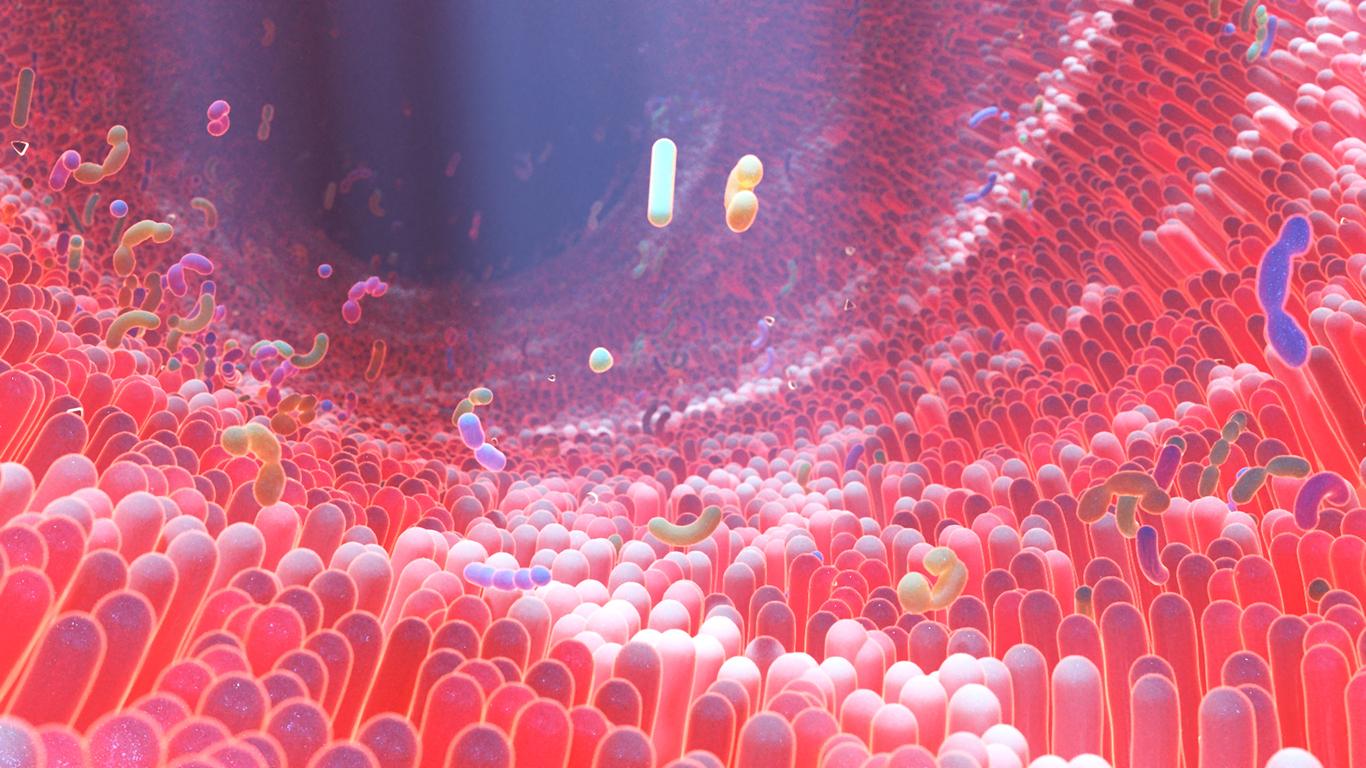
When our intestinal microbiota is weakened, our immune functions are at their lowest. By regaining diversity, this allows our body to better defend itself against aggression.
-1606477617.jpg)
- The strength of our gut microbiota depends on the strength of our immune system.
- The microbiota works hand in hand with the immune system, it is he who is responsible for ensuring the proper functioning of immunity.
The fauna in our guts determines the strength of our immune system. This is how the work of researchers at the Memorial Sloan Kettering Cancer Center (United States) can be summed up in a few words. Grouped in a multidisciplinary team, they demonstrated that the intestinal microbiota and the concentration of different types of immune cells present in our blood shape our immune system. The results of this study were published on November 25, 2020 in the journal Nature.
The intestinal microbiota, also called intestinal flora, represents all the bacteria, fungi and microorganisms that populate the interior of our digestive tract. All this fauna contributes to the good health of our body, because it is essential to ensure functions such as digestion and the synthesis of elements essential to our organism.
Studying the “rebirth” of immunity after cancer
“The scientific community had already accepted the idea that the gut microbiota was important for the health of the human immune system, but the data they used to make this hypothesis came from animal studies.says Joao Xavier, systems biologist at the Sloan Kettering Institute and co-author of the study. In our laboratory, we have a remarkable opportunity to follow how the composition of the microbiota changes in people treated for blood cancers..”
To do this, the researchers used data collected on more than 2,000 patients who had participated in studies on the subject over the past ten years. Their research focused on the different types of immune cells found in the blood, as well as how they evolved, depending on whether or not bacterial strains were present in the gut.
The data used for this study comes from people who have received a stem cell and allogeneic bone marrow transplant. When chemotherapy and radiotherapy sessions are prescribed for a patient to destroy cancerous blood cells, these cells are replaced with stem cells from a donor, in order to make new blood cells.
During the first few weeks, before the donor’s blood cells — including the white blood cells that make up the immune system — are usable by the body, patients remain vulnerable to infections. To protect them, they receive antibiotics to fortify them. However, these antibiotics can have undesirable side effects, in particular by destroying part of the intestinal microbiota. In that time, some strains that are dangerous to our body can settle in to fill the void. When the patient’s immune system has rebuilt, antibiotics are discontinued and the gut microbiota can restart and resume its place in the body.
A diversified microbiota, the key to good immunity
It is the concomitant phenomenon between our microbiota and our immunity that interests Jonas Schluter, assistant professor at Langore Health University Medical Center and co-author of the study. “The parallel recoveries of the immune system and the microbiota, both damaged and then restored, give us a unique opportunity to analyze the associations between these two systems.”
For years, researchers have collected and analyzed stool and blood samples from patients undergoing bone marrow transplants. The database thus created contains details of the types of microbes that live in the intestines of patients at different times. The team then used machine learning algorithms to extract meaningful data from electronic medical records. The data in these records included the types of immune cells present in the blood, information about the medications given to the patients as well as the side effects they experienced.
A previous study published at the beginning of the year already showed that the presence of a great diversity of species in the intestinal microbiota was linked to a lower risk of death after a bone marrow transplant. Additionally, the presence of low microbiota diversity prior to transplantation has been found to result in a higher likelihood of graft-versus-host disease, a life-threatening complication in which donor immune cells attack healthy tissue.
.