Adding papillomavirus screening to conventional smears improves the efficiency of the examination. More precancerous lesions are identified with this method.

“From 25 to 65 years old, a smear every three years. The recommendation is well known to French women. Indeed, this examination makes it possible to detect precancerous lesions of the cervix. But it would have every interest to evolve, according to an Australian study. Posted in PLOS Medicine, she confirms that including a screening test for the human papillomavirus (HPV) makes it possible to better identify the warning signs of cancer.
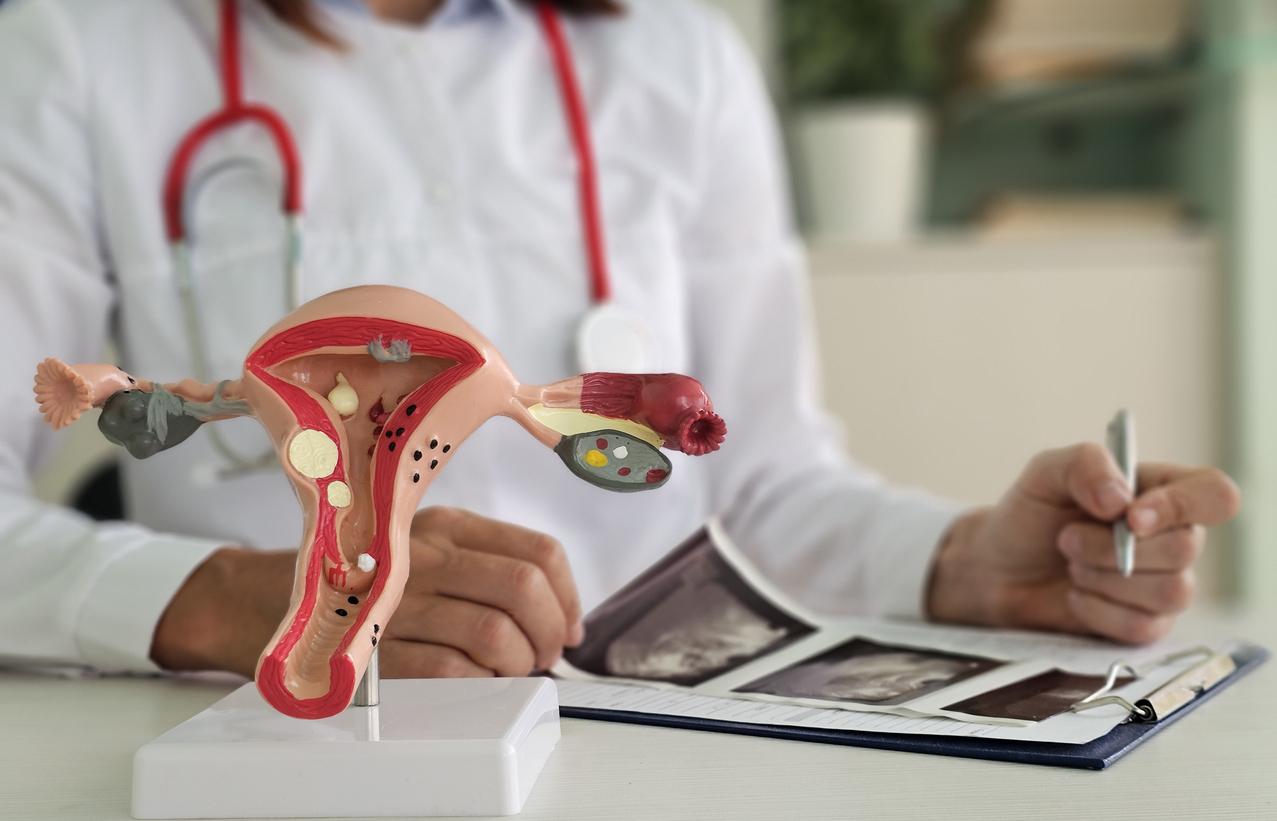
Currently, the screening smear works the same everywhere. Cells are taken from the cervix and then analyzed. Lesions are looked for. But this method has a limit: the presence of the papillomavirus is not measured. However, a persistent infection is responsible for the majority of cancers located in this area.
A more efficient test
By the end of 2017, Australia will therefore change its method. In addition to the classic smear, routine exams in women over 30 will include HPV testing. This work, carried out in New South Wales, confirms the interest of this decision. In fact, its effectiveness has been demonstrated for several years.
In a national study, nearly 5,000 women tested several screening methods. Aged 25 to 65, they were divided into three groups; some received a classic smear, others a smear supplemented by an HPV test using two different approaches.

The conclusion is clear: include research for the human papillomavirus in the routine exams Is usefull. More precancerous lesions are identified. Where the usual smear detects only 0.1% of abnormalities, the HPV test detects 1%. “These results confirm the better performance of HPV screening compared to cervico-uterine smear in a vaccinated population,” concludes Dr. Karen Canfell, first author of the study. Identifying a persistent infection also helps to strengthen surveillance.
One smear
The preventive vaccination of participants is the real novelty brought by this study. Australia is known for its strong coverage via Gardasil. But the version currently on the market protects against two oncogenic strains of the papillomavirus … while at least around twenty are identified.
It is for this reason that smears are still performed: they do not replace regular screening. This “will continue to be necessary insofar as the first generation vaccines protect against the strains involved in 70% of invasive cancers of the cervix”, explain the authors.

Logistically, combining the two exams will not have much impact on women. Indeed, the search for the papillomavirus can be carried out on the same sample. The problem is that this exam is poorly followed in France. Currently, only half of women follow national recommendations.
According to the National Cancer Institute (INCa), carrying out a regular smear on the entire population could prevent 9 out of 10 cancers. The health agency therefore plans to set up organized screening, as in the prevention of breast cancer.
.