Up to what age can an ablation be performed as part of the treatment of atrial fibrillation? This is a question we asked Professor Pierre Jaïs, cardiologist and rhythmologist at the Bordeaux University Hospital, on the occasion of Atrial Fibrillation Week 2022.
- In France, it is estimated that atrial fibrillation affects four people out of 1,000, or approximately 250,000 individuals.
- This disorder must be taken care of quickly because it can lead to many complications including stroke.
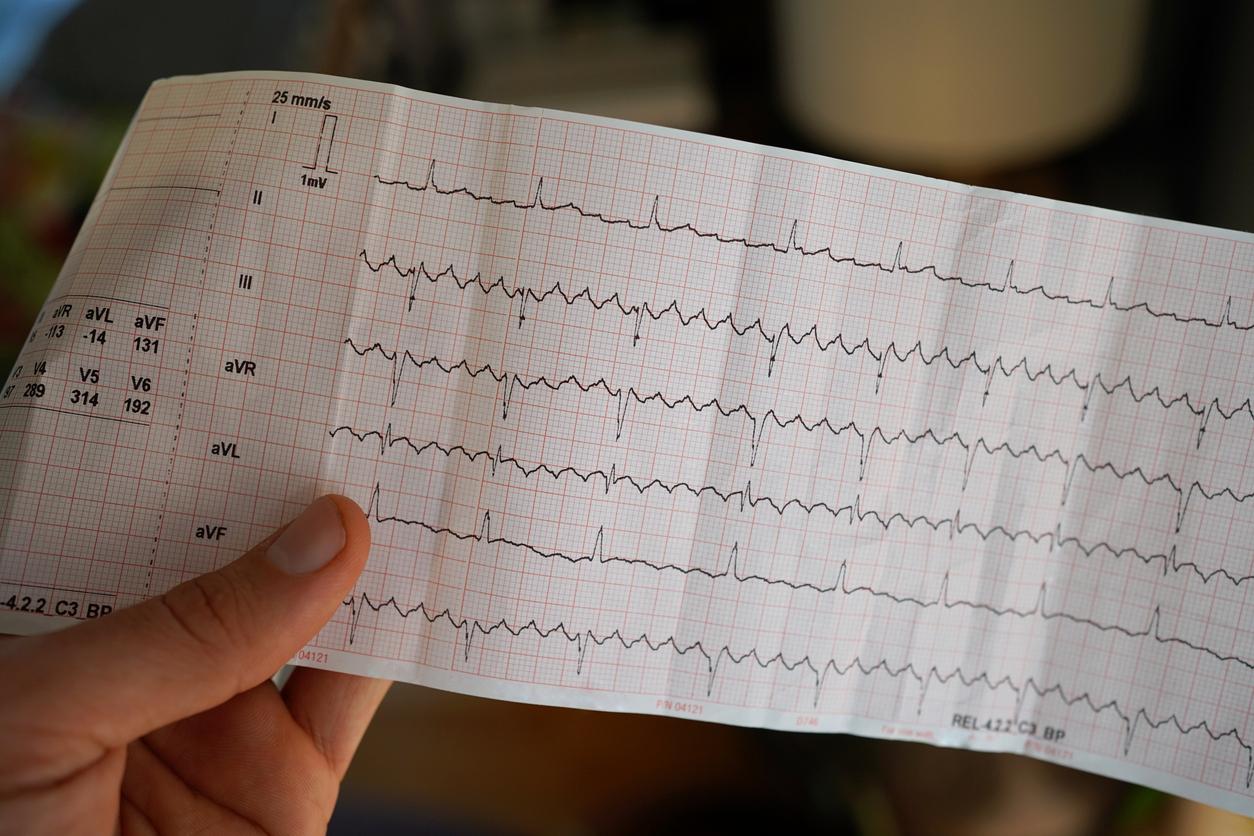
- Taking anticoagulants and atrial ablation are among the possible treatments. This second technique consists of destroying or isolating areas of tissue at the origin of the arrhythmia.
After analyzing the risk-benefit ratio of anticoagulant treatment in patients suffering from atrial fibrillation with Dr Xavier Waintraub on Monday, the question of ablation with Pr Pierre Jaïs, cardiologist and rhythmologist at the Bordeaux University Hospital, and director from the Institute of Rhythmology and Cardiac Modeling.
An “underuse” of ablation with only 3% of patients treated
In atrial fibrillation, we now have a technique called ablation, which is reaching maturity. At present, what can we expect from it?
Ablation has existed for a long time in the form we know, that is to say essentially the isolation of the pulmonary veins. This is something we have been doing since the early 2000s, or even a little before, and which is now part of international recommendations. The best indication is patients who are symptomatic and for whom at least one anti-arrhythmic has failed, which ultimately makes a lot of people.
We must of course take into account the physiological state of the patients, but we are not at all in an excess of ablation, we are on the contrary in an underuse of this technique, undoubtedly for lack of access to interventions that still remain somewhat complex. We currently treat about 3% of patients who have atrial fibrillation, which is most certainly a major underutilization, even though we know that it works better than anti-arrhythmic drugs… So we have a lot of progress to be made at this level.
With the traditional technique of ablation, what are the current “good indications”? And in particular until what age can this technique be practiced?
The question of age is always a relevant question when it comes to an intervention, because ablation is a form of aggression. That said, it has been shown that it is not, in terms of comparison with anti-arrhythmics, something more dangerous or giving more side effects. These can be serious, although Cordarone® can also give serious side effects. So on average people are between 50 and 60 when they have an ablation, but the extremes are very wide. The youngest patient for whom I intervened was 16 years old: he is a cyclist and was very embarrassed by this fibrillation. The oldest must have been 86 years old. Of course, I am not saying that it is necessary to intervene in all octogenarians, it depends on their physiological state, but it should not be hesitated to do it when they are otherwise in good shape and bothered by arrhythmia.
“You have to have a life expectancy of more than a year for it to be justified”
In particular, there is something in the indications that does not necessarily immediately come to mind. It is patients who have “Brady-Tachy” syndromes, with disease of the sinus, who can really benefit a lot from the intervention. That is, sometimes what bothers them the most are the breaks in the reduction of bouts of fibrillation. And as the anti-arrhythmics aggravate this phenomenon, the fact of being able to suppress both the fibrillation and the treatments allows them quite often to avoid the installation of a pacemaker. So we don’t have an age limit as such, but it’s obvious, and it’s also in the recommendations, that you have to have a life expectancy that exceeds one year for it to be justified.
Electroporation: a “revolution” that reduces the risk of side effects
We are now seeing the emergence of new ablation techniques that are a little less aggressive, with fewer side effects. Does this risk modifying the indications for ablation?
Indeed, we lived for 30 years with radiofrequency, for 15 years with cryotherapy which was also in competition with radiofrequency, without any of the randomized trials having demonstrated the superiority of one over the other. . And in recent years, we have had a revolution called electroporation or “pulsed field ablation”. It’s a revolution because we actually have a much lower risk of side effects.
There is also a fascinating aspect to this energy which is called “tissue specificity”. This means that when the electric field which is intended to kill the cardiac cells which we want to eliminate because they are responsible for the arrhythmia, is applied in a rather broad way, if it includes for example the nerve phrenic or esophageal cells, we will not create permanent damage to the phrenic nerve. So we don’t have long-term phrenic paralysis, and it looks completely harmless on the esophagus. However, one of the complications that scares us the most with radiofrequency ablation is precisely the atrio-oesophageal fistula which is accompanied by 60 to 80% mortality. And when the patients do not die, they have after-effects which are sometimes heavy and consequent. So, electroporation and its organ specificity is really a big step forward in terms of the safety of the gesture, even if once again, it concerns few patients. And at the same time, it seems that we have less induced lesions on the pulmonary veins which are more durable than what we knew with radiofrequency and cryotherapy. So it’s really very interesting. The icing on the cake, it’s easier to use and it goes faster! This is something important when you want to scale up and treat more patients.
“This disorder is not sudden death, it is an undermining of the body and the brain”
To conclude, what is your message for the confreres and the sick?
Ablation is a good solution for symptomatic fibrillation that is resistant to at least one antiarrhythmic. Finally, almost whatever the age, if the indication is strong, we will be able to perform the gesture. So that’s important.
Moreover, I think that currently we do not yet have enough recourse to ablations. And finally, my third message is to say that when you have persistent forms of fibrillation, you shouldn’t wait before sending the patient to consult an electrophysiologist to find out whether or not it’s a good indication to perform an ablation, because that there is a loss of chance when one waits. Ablation before six months of uninterrupted fibrillation gives good results. Beyond a year, it deteriorates. And it’s heartbreaking for me to receive patients for whom fibrillation has been permanently installed for a year, two years, three years, five years. And even if the symptoms are not very strong at the start, it should be known that the fact of not evaluating the possibility of an ablation early on is ultimately to amputate the patient’s chances in the longer term. Indeed, we know that this atrial fibrillation is associated with more dementia, more death or even more kidney failure. This disorder is not sudden death, it is an undermining of the body and the brain. It really is something that is much worse than sinus rhythm. And so ultimately, you have to be very careful when you make the decision to respect persistent fibrillation.