Botox, Medicines and Surgeries
Many women with bladder or prolapse symptoms find it difficult to talk about their problem. Seeking help is therefore too rare. And that while there are all kinds of different treatment options. Professor of urogynaecology Huub van der Vaart talks about the options.
“The pelvic floor problem is a very broad field. The treatment depends on the complaints. The possibilities are in full development.
Stress incontinence
At the moment, all guidelines state that the treatment of someone with urine leakage with exertion (stress incontinence) begins with pelvic physiotherapy. However, from the UMC Utrecht, together with 20 hospitals and 50 physiotherapy practices, we have conducted a very large study into the treatment of people with moderate or severe incontinence. In patients with severe stress incontinence, direct surgery appears to be much more effective than physiotherapy. In the long run, it is also associated with lower costs.
During the operation, a plastic band is placed under the urethra. This is done with an epidural or under a short anesthesia. Usually the patient can go home the same day. The operation is very effective: 85 to 90 percent of the women are dry afterwards or lose at most a drop.
Based on our research, we have made a model, with patient characteristics, with which we can estimate which patient benefits from direct surgery and which from physiotherapy. This model will be used more in the future.
Overactive bladder/urge incontinence
Even with an overactive bladder, pelvic physiotherapy often first choice. Physiotherapy is often combined with drugs that inhibit bladder excitability. In general, these drugs work very well. The drugs can have side effects, commonly heard side effects are a dry mouth and difficult bowel movements.
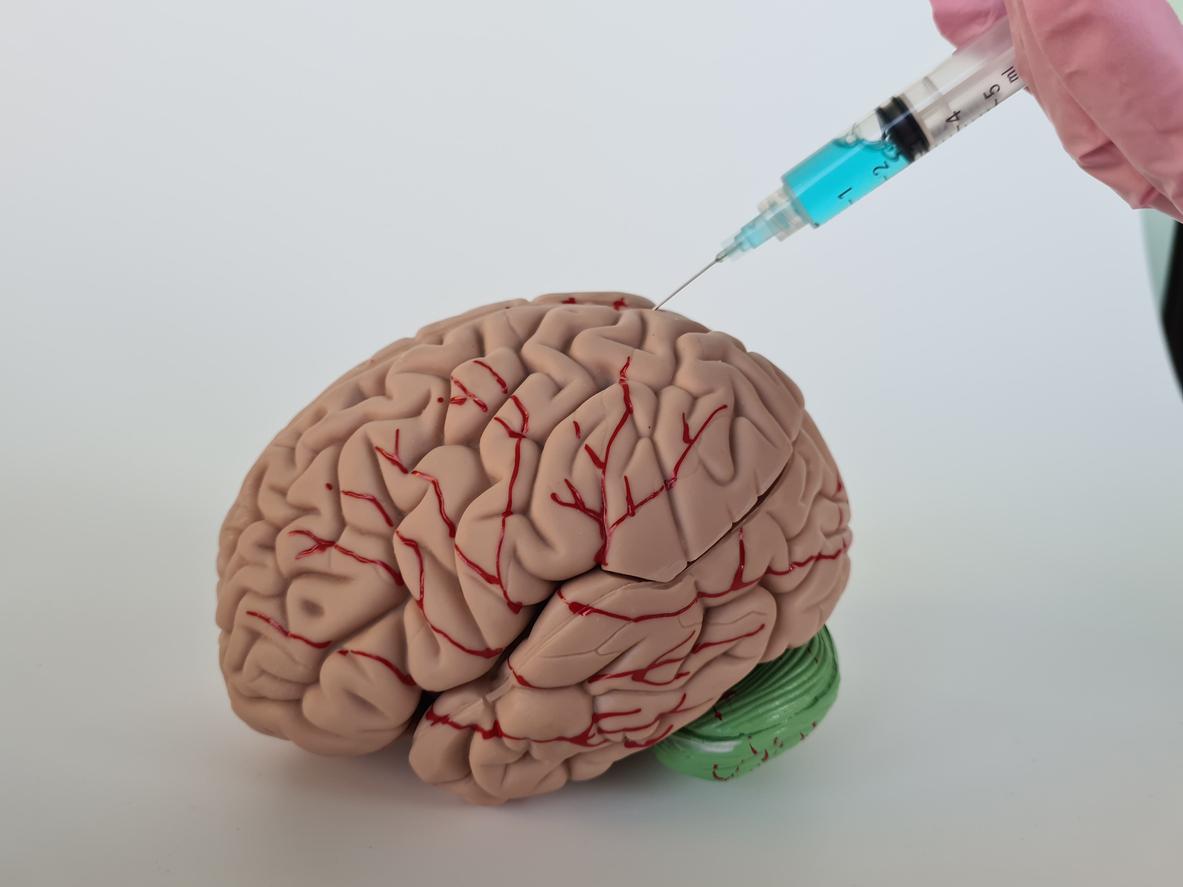
If physiotherapy and medicines together have insufficient effect, we often perform a bladder function test. Based on the outcome, we determine the further treatment. One of the options is a treatment with botox. By partially paralyzing the bladder muscle with botox, women have more time to go to the toilet. We inject the botox on 10 to 20 different spots – after anesthesia of the bladder wall with a gel – so that the women can still urinate.
Another possibility is nerve stimulation. We then place a kind of acupuncture needle in the ankle and stimulate the nerve with it for about 20 to 30 minutes every week. We don’t know exactly how it works, but thanks to this treatment, the bladder becomes less irritable.
prolapse
About the treatment of a prolapse of the uterus, bladder or rectum is currently a lot of fuss. There are also significantly less successful treatment methods in this area.
You can use a vaginal ring if the prolapse is not that far outside the vagina. In combination with pelvic physiotherapy, this can give very good results. Pelvic floor physiotherapy has no proven effect in the case of a significant prolapse.
Surgery is then still an option. Such an operation is successful in three quarters of the women, but unfortunately the prolapse returns in 15 to 30 percent. This does not mean that you will be hindered by this again. We know of two types of operations.
In the classical operation, the connective tissue of the patient is used to remedy the prolapse. We stitch the fabric back together. However, you are dealing with connective tissue that has previously been damaged (and prolapsed) and that becomes of lesser quality with age. That is why the operation is not always successful or the effect is not permanent.
mats
That is also the reason that plastic mats are used in the other operation. These pads – made of the same material as the strap under the urethra – provide extra support to the bladder, uterus or rectum if they have prolapsed.
Unfortunately, unlike the band under the urethra, the operation with a mesh is associated with a risk of complications. Some patients have persistent pain after insertion of the mat. This is extremely annoying because there is often little that can be done about it. The mat can also irritate the vaginal wall and cause discharge. Fortunately, the latter is often good and easy to remedy.
For these reasons, a lot of research has been done on this operation. The professional association of gynecologists has taken a position in this area and has drawn up a guideline. The mats may only be used on women who have already had one or more classic operations that were unsuccessful. Clear safety requirements are now imposed on the gynaecologists and clinics that use the meshes. There are also different types of mats on the market; the risk of complications varies by species. Information for women is therefore of great importance: women must be aware of the advantages and disadvantages.
Compared to patients with chronic pain complaints, there are also many patients who are very happy after placing the mat because they have got rid of their prolapse. The quality of the mats is improving and gynecologists also know better and better how to perform the operation. More experience gives better results, so feel free to ask as a patient about the experience a doctor has.”
Professor Dr. Huub van der Vaart is co-founder and medical director of the Women’s Care division of Bergman Clinics, formerly Alant Vrouw. They have two locations in Amsterdam and Bilthoven, where they provide multidisciplinary care for women with pelvic floor problems. There is close collaboration with the University Medical Centers in Amsterdam and Utrecht. He is also head of the department of reproductive medicine & gynaecology at UMC Utrecht. In February 2012, he was appointed professor of Urogynaecology by Utrecht University.