A new study explains the deaths of newborns with sepsis: commonly used antibiotics are no longer effective against this bacterial infection, formerly known as sepsis.

- Antibiotic resistance is responsible for the death of newborns with sepsis.
- This observation concerns more low-income or middle-income countries.
- Doctors were forced to give antibiotics as a last resort.
The mortality rate varies between 1.6% and 27.3%, depending on the hospital where newborns are cared for for their sepsis. This is the result of a study published in the journal PLOS Medicine. During this work, the researchers also discovered that nearly one in five infants worldwide die from this bacterial infection… and these deaths are largely linked to antibiotic resistance.
Sepsis: antibiotic resistance responsible for newborn deaths
For their study, the scientists collected, between 2018 and 2020, data from more than 3,200 newborns with sepsis in 19 hospitals in eleven countries (Bangladesh, Brazil, China, Greece, India, Italy, Kenya, South Africa , Thailand, Vietnam and Uganda). Results: the deaths of babies are linked to antibiotic resistance, ie the fact that the antibiotics used are no longer as effective in fighting bacteria. Mortality rates were higher in low-income and middle-income countries.
“Organisms evolve, drug resistance changes. This is why clinical guidelines for neonatal sepsis must be constantly adapted, explains Dr. Wolfgang Stöhr, one of the authors of this work. This observational study is an important step towards better treatment.”
The objective is to provide elements to the World Health Organization (WHO) to improve guidelines for the treatment of newborns with sepsis. Indeed, the publication of this study is part of a context of increasing cases of severe sepsis associated with a new variant of an enterovirus in infants in France. As of May 5, out of nine cases, seven had died and two were still hospitalized in the neonatal unit according to a press release from the World Health Organization (WHO).
“The study revealed the stark reality of antibiotic-resistant infections, particularly in hospitals in low- and middle-income countries, where we often face shortages of nurses, beds and space, says Professor Sithembiso Velaphi, one of the authors. The risk of infections is very high and most infections are resistant to antibiotics. If an antibiotic does not work, the baby often dies. This needs to change urgently. We need antibiotics that will cover all bacterial infections.”
Sepsis: antibiotics of last resort to treat the infection
If these results are worrying, it is also because more than 200 different antibiotic combinations were used by the hospitals in the study, with frequent changes of antibiotics due to the high resistance to the treatments. This means that not just one class of antibiotics is affected by antibiotic resistance, but a whole panel.
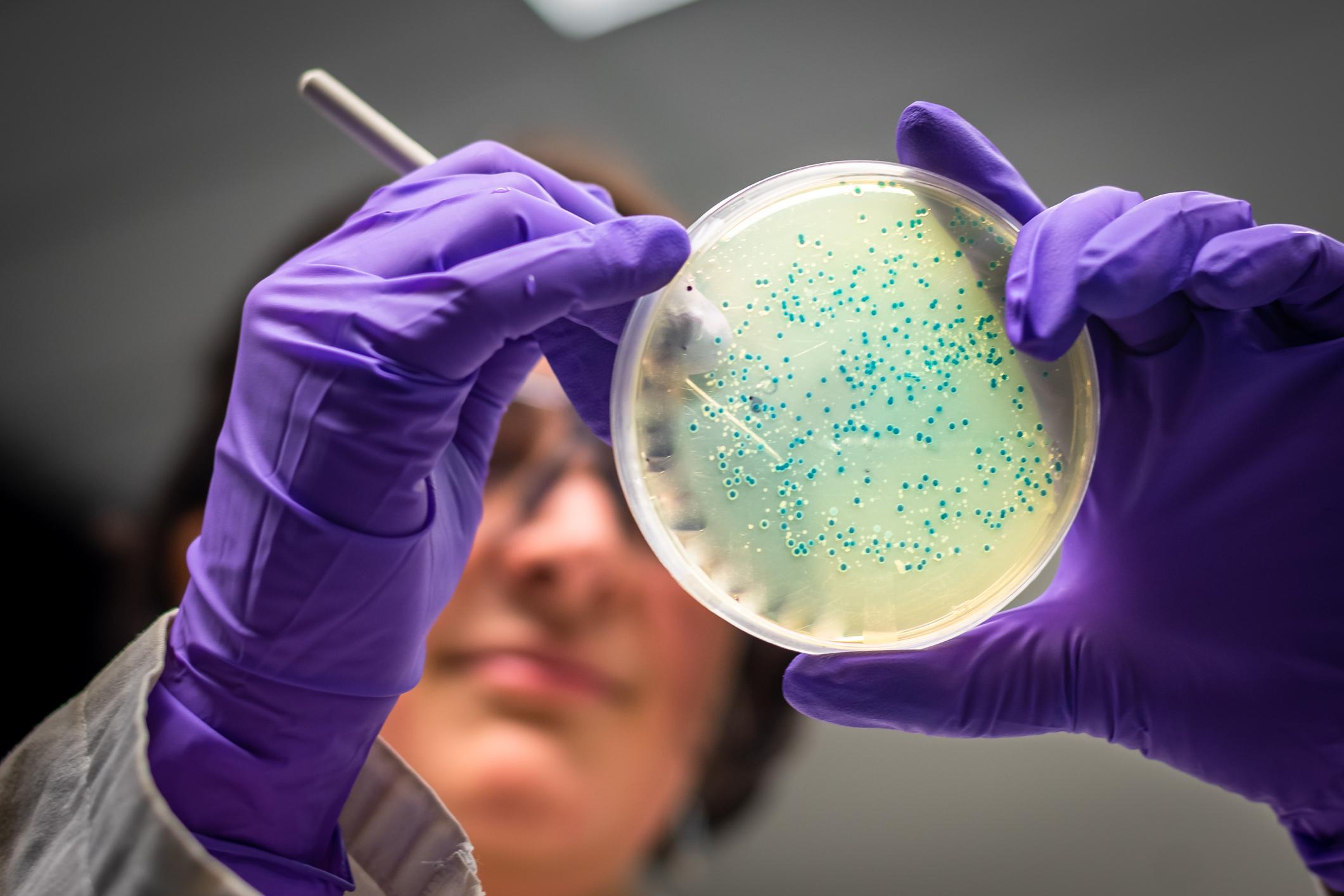
Because of this antibiotic resistance, several doctors in the study also had to use antibiotics of last resort, such as carbapenems which, according to the High Authority for Health (HAS) “be limited [au] hospital environment to serious nosocomial infections and/or due to multi-resistant bacteria on microbiological documentation.“In the study, 15% of babies with sepsis received last-line antibiotics.
Klebsiella pneumoniae [qui peut être à l’origine d’un sepsis] was the most common pathogen in newborns in the study. It is an enterobacteria that the WHO has placed at the very top of its list of bacteria against which it is urgent to have new antibiotics. “These bacteria [Klebsiella pneumoniae et d’autres] have become resistant to a large number of antibiotics, including carbapenems and third-generation cephalosporins, the best products available for treating multidrug-resistant bacteria.”