(you have to dare)
In the past, the pain threshold was sacred to doctors. Now they know that sometimes you have to hurt someone a lot to get rid of their chronic pain. Where does this shift in thinking come from?
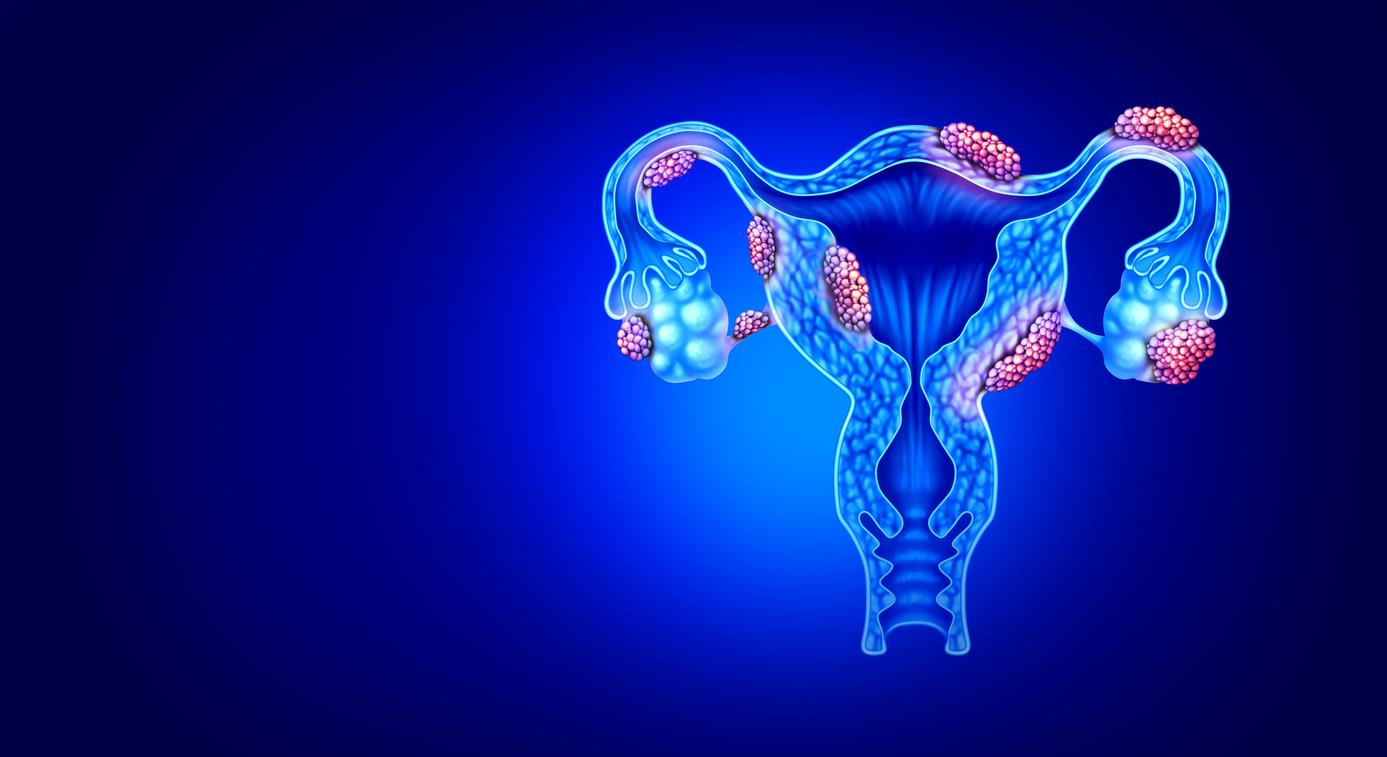
“You won’t need that wheelchair anymore,” said the taxi driver who took Ricky van der Pijl (51) and her husband to a remote mountain village in Macedonia on a sunny April day. She had not been able to walk for four years. She suffered from CRPS (Complex Regional Pain Syndrome), a condition she contracted after an accidental fall from a truck. Since then, her foot had been red and swollen. She flinched in pain at the slightest touch.
She had followed all possible treatments and pain therapies, but nothing helped. “You are out of treatment,” doctors had said. At her husband’s urging, she decided to make one more attempt at Mrs. Shinka, a Macedonian who was said to have special gifts. Mrs. Shinka, a woman dressed in black in slippers, took her aching foot without hesitation and did what no doctor should have done to Ricky: she started squeezing it. Pop, pop, pop, Ricky heard. Even though she was in pain, Mrs. Shinka kept going. “You’re going to walk down this red carpet now,” she instructed Ricky moments later.
Operation without knives
Ricky: “It was unbelievable. The pain made me cringe, but I walked!” The treatment was repeated for five days. On the third day, Mrs. Shinka squeezed so hard that Ricky passed out. “It was like surgery without knives. When I came to, I knew I was cured.” At the end of the week, she climbed two hundred stairs to a monument near the village. Her wheelchair went back home, but now as a luggage carrier for the suitcases: Ricky walked behind it himself. “I’m walking and cycling again and the pain is pretty much gone,” she says five years after her recovery.
No Macedonian Jomanda
She’s not alone. Dozens of Dutch people with CRPS traveled to Macedonia in recent years and came back reborn. This includes some patients of the Hoogeveen GP Jan-Willem Ek and rehabilitation doctor Jan van Gijn of the Bethesda Hospital in Hoogeveen. They found the results so remarkable that they traveled to Ms. Shinka with six patients who had finished treatment.
Ms. Shinka was not a Macedonian Jomanda, they concluded after further investigation. She deliberately applied a method that went directly against the usual treatment in the Netherlands: instead of staying within the patient’s pain threshold, she went right through it.
Contrary to what doctors and patients have long thought, sometimes it’s good not to care about pain. “With CRPS, it is many times more effective to move the affected limbs directly, without taking the pain into account,” says rehabilitation physician Eveline Maring of Bethesda Hospital. Since 2003, the Hoogeveen hospital has treated more than five hundred CRPS patients in this way, inspired by Mrs Shinka. In the beginning, the rehabilitation doctors were viewed with suspicion by colleagues from other hospitals. But the results are so good that twenty other rehabilitation centers and rehabilitation departments of hospitals have adopted the method.
Out of the wheelchair
After being diagnosed with CRPS, Maring explains to her patients why they are in so much pain. “Your body is like a house where the alarm has gone off after a break-in. The alarm still goes off, but there is no intruder anymore. The pain you feel is no longer useful.” She then explains what the treatment entails: with physiotherapy move the sore body part.
Every time she is delighted when someone gets out of their wheelchair after three or four weeks. “That happens regularly. If I didn’t see it with my own eyes, I would have a hard time believing it.”
How does the patient’s family react to such a cure? Maring: “The danger is that it will downplay the condition. ‘If you get better so quickly, it must have been nothing.’ That is why we always invite the partner to the treatment, who must see with their own eyes how much pain it costs.” Not everyone dares to do it. Maring: “Some people have completely adapted their lives. They have other work or a disability benefit, they play wheelchair tennis. They all put that at risk. I can well imagine that they are afraid of that.”
She cannot guarantee that everyone will get rid of their pain. But nine times out of ten, treatment does restore function to the affected body part, Maring says. “In half of those patients, the pain also disappears completely or partially.” According to her, there is hardly any relapse, but that has yet to be scientifically proven. This autumn, the results of the first study into the long-term effects of the treatment, conducted by Radboud University, will be announced.
A new message
“A large part of our members is wary of the Macedonian method,” says Elly Roetering of the Pain-Hoop Foundation, a patient association of people with chronic pain. “Their great fear is that the pain will get worse. They do not dare to take that risk. Especially not as long as it is not conclusively established that this method works. We also hear stories from people for whom it has not helped.”
Jos van der Geest (63) wakes up every day with pain in her neck and shoulders. Nineteen years ago, after a collision, she received a whiplash. She can well imagine that many CRPS patients are reluctant. “Whether the Macedonian method also works for whiplash is unknown. But if it did, I don’t know if I would try it. It took me years to learn to live with the pain. I now know what I not what I get back after such treatment.”
After years in one hospital and out of another, she decided to turn her back on the medical circuit. “The pain is always there and will never go away. The thought that I can handle it keeps me going.” She runs her own drugstore four days a week. “I live by strict rules, so I can continue to work.” That means up every morning at seven o’clock relaxation exercises to do, rest at noon and go to bed at seven o’clock in the evening. Her pain threshold hasn’t changed, she says. “I’ve learned to put up with it. Sometimes I say to myself: Please sit in my big toe. It doesn’t make sense, but then I can take it again.”
Courage
“It takes courage to participate in a treatment that goes beyond the pain threshold,” says Maring. “People need to rely completely on practitioners who have a new message: move despite the pain, rather than rest and be careful.”
hereditary
The Macedonian method marks a complete change in thinking about pain. It used to be thought that pain was caused by damage to body tissue (a wound, inflammation, twisted vertebra). If it was not found, the pain would be ‘between the ears’.
“In fact, that statement is correct,” says neuroscientist and pain expert Ben van Cranenburgh of the Institute for Applied Neuroscience. “But it suggests that real and not real pain would exist. Pain sensation always originates in the brain. And whether pain is caused by tissue damage or not, for the patient that pain is reality.”
Brave or petty are words that are not in his dictionary. “The pain threshold, i.e. the moment you feel pain, is about the same for everyone. Everyone feels pain when they put their hand in a bowl of hot water.”
What does differ is how the brain responds to such a painful stimulus. And that has everything to do with sensitivity of the pain system in the brain. Van Cranenburgh: “This is partly genetically determined: the brains of some people recognize pain stimuli earlier and will experience pain more intensively.”
Only after 1980 it became clear through brain research that the pain system can change drastically in the course of life. Van Cranenburgh: “Because of illnesses and injuries, or for example due to a difficult delivery, the pain system can become more sensitive. But thoughts about pain also have an influence. In someone who thinks: it will pass, the pain system develops differently than in someone who is immediately concerned if he feels something suspicious.” These brain changes can be the cause of certain types of chronic pain that persists after healing. Lower back pain, fibromyalgia or CRPS for example.
Vicious circle
In addition to long-term changes, there are rapid changes in the pain system. Whether and how much pain someone feels is highly dependent on the situation. It is no exception that a runner with a sprained ankle finishes the marathon. If that same runner gets lost during a walk with his grumpy father-in-law, he may not be able to move a step. Van Cranenburgh: “At that moment he really feels a lot more pain.”
Fear also plays a role. “With concrete fear, for example if you are threatened with a knife, the pain threshold rises and the pain decreases. Survival then has priority over the pain. When it comes to indefinable, vague fear, the sensitivity to pain increases. open all senses to get more clarity.”
When done right, pain warns of possible damage in the body. But pain can also turn against you: the pain system in the brain can go into overdrive. “That is probably the case with CRPS. People get caught in a vicious circle,” says the pain expert. “They think: I have something on my leg. If I move it, the pain gets worse. Because of that inactivity, the brain no longer receives signals about that leg. As a result, the corresponding brain area becomes more and more sensitive. Better a painful leg than a numb leg , the brain thinks, as it were.”
Normal feedback
The insight that chronic pain often involves changes in the brain is gaining ground. Van Cranenburgh: “That means that the treatment should focus less on the area where the pain is located and more on the neural pain system. Unfortunately, not all doctors are convinced of this yet.”
According to the pain expert, the neural pain system can be ‘reset’ in several ways. By explaining that the painless alarm is for example. By looking for a pleasant environment, watching an exciting movie or listening to beautiful music. Or by moving the painful body part again. “In the latter way, the pain system of CRPS patients can normalize. Just the thought: my leg is for walking on, can take care of that. Then the brain finally gets normal feedback about that leg.” That doesn’t just happen with CRPS. Also people with lower back pain or a hernia are increasingly being advised to keep moving.
Experimental Therapy
At the university hospital in Maastricht, people with chronic pain complaints have been successfully treated with ‘graded exposure in vivo’ for several years now. Also in this experimental therapy, patients have to overcome their fear of pain. They see pictures of actions they no longer dare. Then they should perform the actions they fear most.
crack or acupuncture are based on a different principle, according to Van Cranenburgh: fighting pain with pain. “We think that a kind of battle is being waged in the brain for neural space. They always have to make a choice. By giving it a painful stimulus, you force the brain to choose. Perhaps that also plays a role in what Mrs Shinka does.”
Sources):
- Plus Magazine