Doctors tested a non-invasive ablation technique, stereotaxic radiotherapy, on five patients with refractory and high-risk ventricular tachycardia. All have seen the number of tachycardia episodes decrease.

Treating ventricular tachycardia by external radiotherapy and without fitting a catheter and electrode into the heart: it is this method that has been tested with incredible success by American researchers. The results are published in the journal The New England Journal of Medicine.
Trials were conducted on five patients with high risk refractory ventricular tachycardia. This method has a considerable advantage: it is non-invasive and allows patients to be treated while they are still awake.
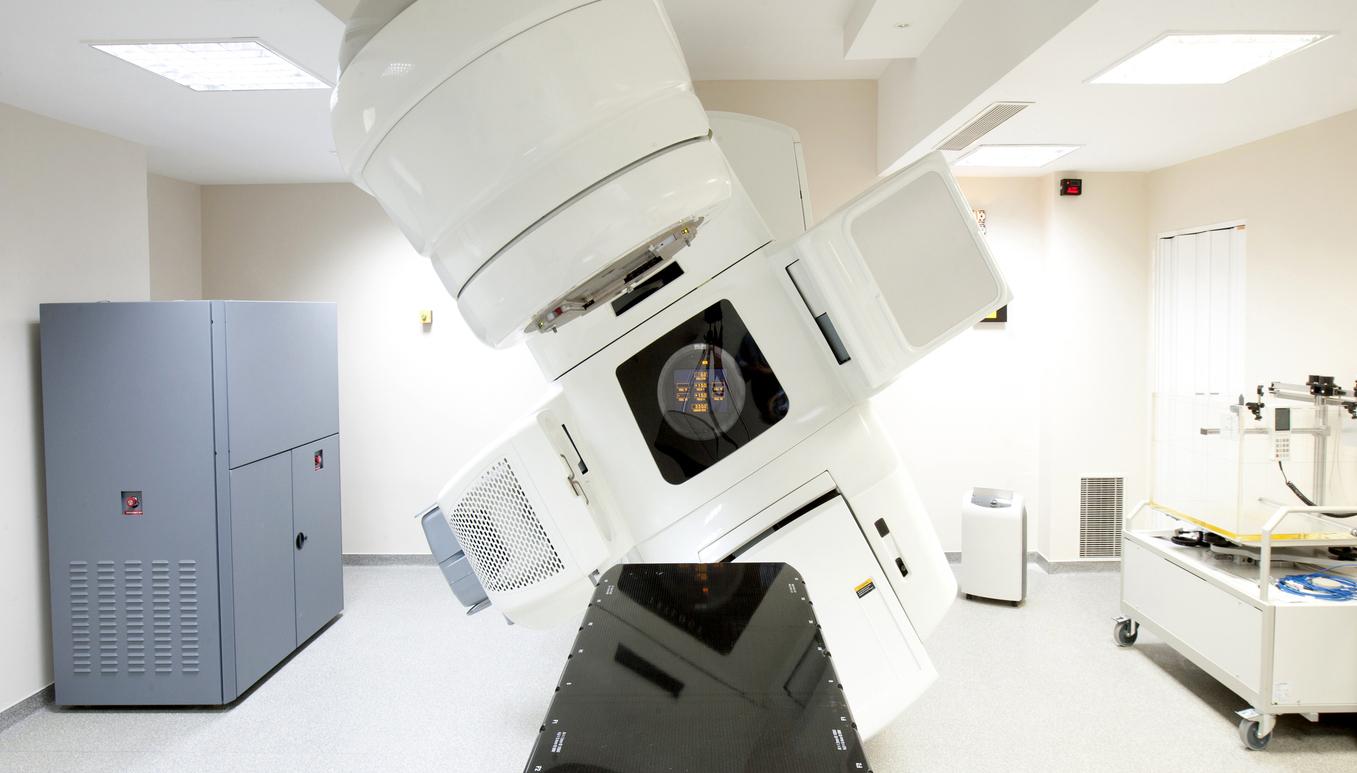
A stereotaxic radiotherapy technique
The challenge was to identify the exact area in the heart where the lesions of the cardiac ventricle are found, causing arrhythmias, generally post-infarction scars or in the context of cardiomyopathy. Their location involves a scanner and an EKG using a jacket with 256 electrodes.
All this allows extremely precise 3-dimensional identification of arrhythmogenic zones. The researchers then used stereotaxic radiotherapy which allows gamma rays to be administered externally, a radiotherapy developed in neurology and which very precisely targets the diseased areas on the 3 D marking.
Astonishing results in the five patients
During the three months prior to treatment, all five patients had experienced 6577 episodes of ventricular tachycardia despite all possible drug and non-drug therapy. Stereotaxic radiotherapy was administered to the 5 patients without problem, followed by a six-week blanking period, or post-radiotherapy period, during which arrhythmias can occur due to post-exposure inflammation. During this time, doctors recorded 680 episodes of tachycardia.
99.9% efficiency
After this period of “blanking”, only four episodes of tachycardia were observed during the following 46 months, a reduction of 99.9% compared to the initial baseline value!
At 12 months, 3 patients are still alive without arrhythmia and without anti-arrhythmic drugs. The five patients therefore saw the number of tachycardia episodes drop drastically. The researchers noted, however, that the lungs may have opacities corresponding to mild inflammation. These resolved after a year.
These results, although preliminary because they relate to only 5 patients with a limited evaluation in time, are extremely interesting in a disease which is usually fatal and whose rhythm disturbances are both a marker of the severity of the heart disease, but also of worsening of heart function
.