A new type of vaccine against pneumonia, called liposome, offers the hope of combining good efficacy with very wide coverage.
Antibiotic resistance is like a war. On the one hand, humanity. By developing antiobiotics, it has managed, in less than a century, to drastically reduce the number of deaths due to infectious diseases. On the other hand, bacteria: under pressure, they mutate and develop mechanisms of resistance to antibiotics. A real arms race, where humans have no interest in falling too far behind.
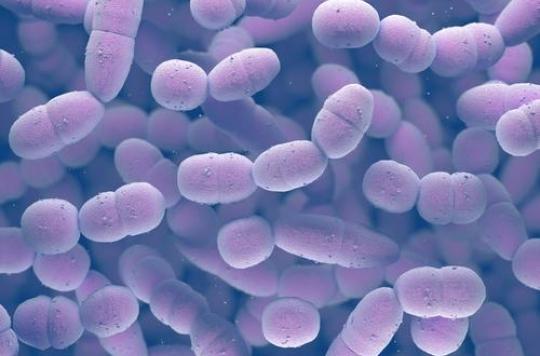
It is with this in mind that researchers at the University of Buffalo (New York) are working to develop a new vaccine against pneumonia. Responsible for the death of a million children per year (WHO, 2015), pneumonia is mainly due to a bacterium: the pneumococcus (S. pneumonia). For the time being, the vaccines available provide the best protection against 23 strains of pneumococci, among the most virulent.
Wide coverage, good efficiency
But it is to be feared that non-targeted strains will proliferate, or that new antibiotic-resistant strains will emerge. However, existing vaccines have limited performance. Polysaccharide vaccines (Pneumo-23, Pneumovax) have a fairly wide coverage but a reduced efficacy, almost zero before the age of two years. As for conjugate vaccines (Prevnar-13), they are more effective but their coverage is narrower (13 strains).
The new vaccine developed at the University of Buffalo, called liposome, aims to combine high efficiency and wide coverage. Tested in animals, it was able to elicit a vigorous immune response against 72 strains of pneumococcus.
Liposome vaccine
Unlike conjugate vaccines, which must combine each target antigen with a carrier protein, liposome vaccines encapsulate all of the necessary antigens in tiny spheres (liposomes), capable of amplifying the immune response on their own. It is therefore much easier and less expensive to add new strains as the need arises.
“Traditional vaccines completely destroy target bacteria,” says Charles H. Jones, co-author of the study. “But with this new vaccine in development, we can monitor bacteria and attack only if they are breaking out of the microbiota to cause disease. This is important because by leaving non-harmful bacteria alone, we are preventing other harmful bacteria from taking their place. “
It remains to test and validate this prototype in humans and, in the event of positive results, to industrialize its production. It will take many more years to come to any eventual finished product, but it is the hope of a new weapon in the frenzied race between man and his tiny hosts.
.