Taking care of your oral health is more effective than using antibiotics in preventing infective endocarditis, a heart infection caused by bacteria in the mouth, according to a new study from the American Heart Association.

- Oral hygiene is as important as taking antibiotics to prevent the risk of infective endocarditis.
- However, antibiotics remain essential before certain dental procedures, in particular in 4 categories of patients at risk defined by the American Heart Association in its new guidelines.
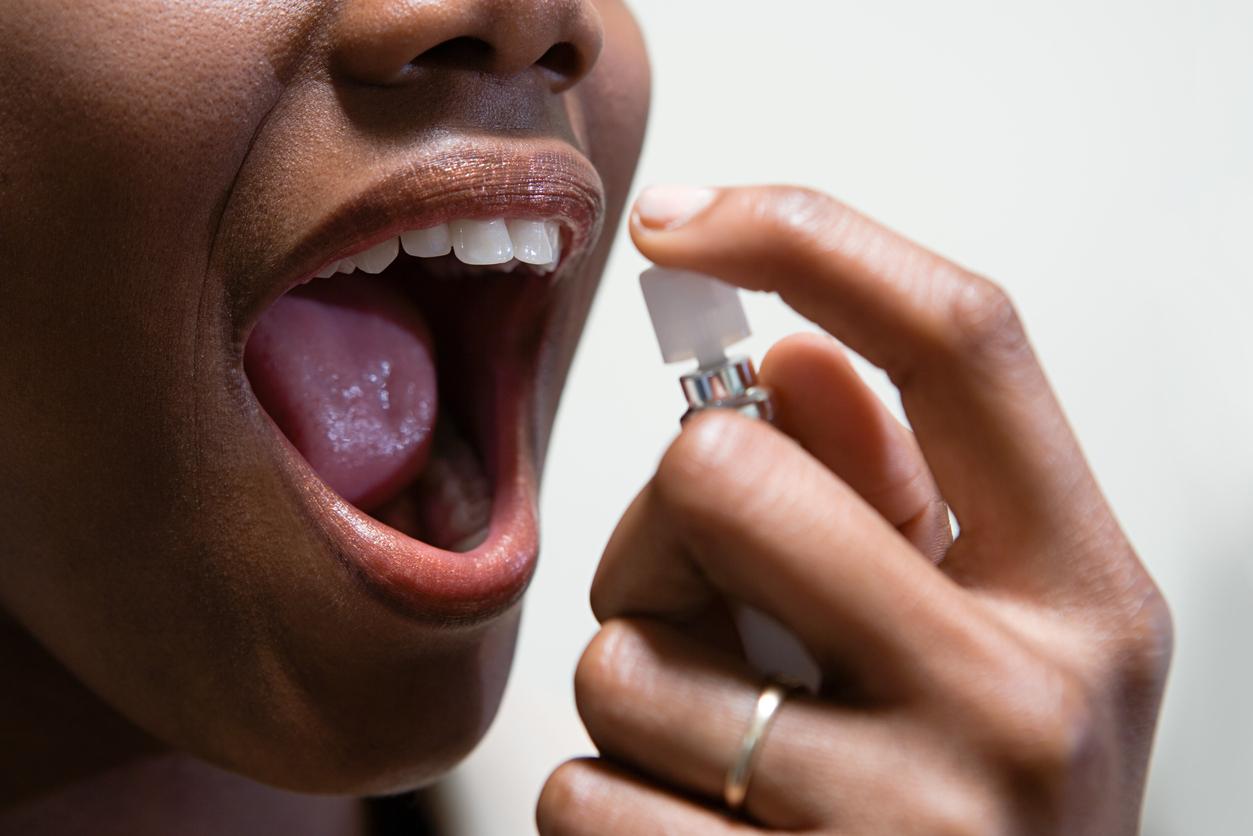
Brushing your teeth at least twice a day, using dental floss and going to your dentist every year does not only help to preserve your smile. This also drastically reduces the risk of infective endocarditis. This heart inflammation is caused by oral bacteria that enter the bloodstream and settle in the inner lining of the heart’s chambers (the endocardium), mainly affecting the heart valves or blood vessels. Streptococci and staphylococci occupy the first place of the offending bacteria: they accumulate in the dental plaque on the surface of the teeth and cause inflammation and swelling of the gums.
Patients at high risk of endocarditis
While poor dental hygiene increases the risk of developing infective endocarditis, some patients are at higher risk. That’s what new guidelines from the American Heart Association highlight. Published in the journal Traffic, they confirm previous recommendations. According to these, there are four categories of heart patients who should be prescribed antibiotics before certain dental procedures to prevent endocarditis, due to their higher risk of infection-related complications. This is the case for patients with prosthetic heart valves or prosthetic materials used for the repair of the valves, those who have already had infective endocarditis, adults and children with congenital heart disease and people who have undergone a heart transplant.
A decrease in the prescription of antibiotics
These new guidelines from the American Heart Association follow those from 2007, which strictly defined which patients should receive preventive antibiotics before certain dental procedures in these four high-risk categories. This change reduced the number of patients requiring antibiotics by approximately 90% and thus limited the overconsumption of antibiotics in the population. These guidelines also did not increase the occurrence of endocarditis or death related to heart inflammation.
Since the guidelines were adopted in 2007, American Heart Association scientists have found an overall reduction of about 20% in the prescription of preventive antibiotics in high-risk patients, a 64% decrease in patients at moderate risk and a 52% decrease in patients at low or unknown risk.
However, in a survey of 5,500 dentists in the United States, 70% of them said they prescribe preventive antibiotics to their patients even though the guidelines no longer recommend it, most often for patients suffering from mitral valve prolapse and five other heart conditions. Dentists reported that in 60% of cases the antibiotic regimen was recommended by the patient’s doctor, and in one-third of cases it was in accordance with the patient’s preferences.
Good oral hygiene to limit the risks
What do these new directives bring, compared to those of 2007? They therefore insist on the need to maintain good oral hygiene and regular access to dental care to prevent the onset of infective endocarditis, and thus further limit the use of antibiotics before certain dental procedures.
“It is important to connect patients with services that facilitate access to dental care and insurance assistance for dental coverage, especially in patients at high risk of endocarditis,” the experts write. of the American Heart Association, which recommend the priority use of preventive antibiotics “in high-risk patients undergoing dental procedures involving manipulation of gum tissue or infected areas of the teeth, or perforation of the membrane lining the mouth”.

.