What is the origin of inflammatory bowel disease (MIC)? According to a team of French researchers from the National Institute for Health and Medical Research (Inserm), the National Institute for Agricultural Research (INRA), the Pierre and Marie Curie University (Paris) and the Public Assistance of Paris Hospitals (AP-HP), the bacteria of our digestive tract and our genes are the main responsible for these pathologies. Their work is published in the journal NatureMedicine.
Abnormalities of the microbiota: “cause and consequence of IBD”
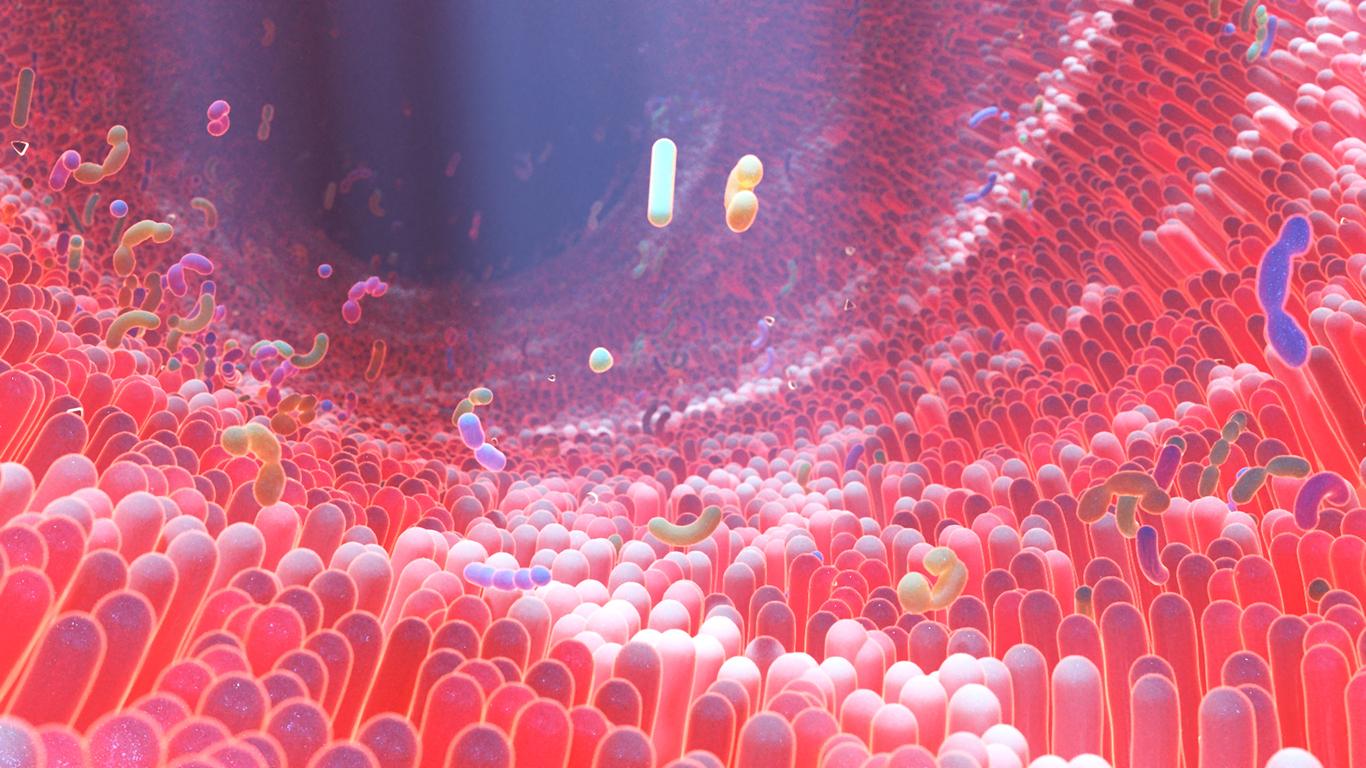
IBD, including Crohn’s disease and the ulcerative colitis, correspond to inflammation of the digestive tract. These diseases have a genetic component already identified before the publication of this new study, but the scientists also suspected the intervention of environmental factors and modification of the gut microbiota(all the bacteria that live in our digestive tract). For this research, the scientists looked specifically at one of the genes involved in IBD, called CARD9. This allows the production of interleukin 22, a protein that participates in the immune recognition of microorganisms. They used mice deficient for this gene, and noticed that in the event of inflammation, the lining of their intestine healed poorly and that the composition of their microbiota was disturbed. After this finding, they transplanted the intestinal flora of these CARD9-deficient mice to other non-deficient mice. Result: these last mice have in turn become hypersensitive in case of inflammation of the intestine. “In other words, the genetic defect in itself is not sufficient to induce the dysfunctions observed. Alterations in the composition of the intestinal flora that results from the absence of CARD9 play a major role in intestinal hypersensitivity and the functional defect of the Interleukin 22 pathway.“explains in a statement Dr. Harry Sokol, hepato-gastroenterologist at Saint-Antoine Hospital (Paris) and head of the study.
But why do bacteria influence the hypersensitivity of the intestine? According to the researchers, these microorganisms fail to produce indole derivatives, which are essential for the production of interleukin 22. And, without interleukin 22, the intestinal terrain is conducive to inflammation. “These results show how all these mechanisms are intertwined; genetics, immune system and microbiota. Thus, microbiota abnormalities in IBD are both cause and consequence of inflammation.” summarizes Harry Sokol.
Towards new therapies
Good news, however: these mechanisms would be reversible. By injecting molecules that mimic indole derivatives into mice deficient for the CARD9 gene, the researchers noticed that the symptoms of inflammation disappeared and that the mice were able to manufacture interleukin 22. It remains to be seen now whether these results are valid. transferable to humans. By analyzing the stools of a hundred patients suffering from IBD, the researchers have already been able to observe abnormally low levels of indole derivatives compared to healthy people, in particular in patients with a mutation in the CARD9 gene. A track that opens the way to new screening and treatment techniques: “we can already very easily identify patients with a defect in the production of indole derivatives from a simple stool analysis. It would therefore suffice to supplement these patients with bacteria producing these derivatives or by administering the derivative in question directly to them.“, suggests Harry Sokol.
>> To read also:
Patients with IBD do not have a good quality of life
Microbiota: a site to learn all about the 100,000 billion bacteria that we harbor
A fatty acid at the origin of Crohn’s disease?
Crohn’s disease: a fecal transplant soon possible?