The Court of Auditors estimates that home hospitalization is making little progress in France. Practical solutions can be implemented to remedy this.

A hospital room fitted out within its own accommodation, and hospital doctors who go to the bedside. This is what home hospitalization (HAD) offers. The idea: to offer the patient a better quality of life while guaranteeing the safety of care and reducing the costs of care. In several countries, such as Australia, home hospitalization quickly established itself as a credible alternative to conventional hospital care.
But in France, this form of care is still struggling to find its patient base. In 2013, the government developed a strategy to develop HAD. Its success remains limited for the moment, as indicated a report of the Court of Auditors, published Wednesday, which gives a mixed assessment of these efforts.
At the hospital as at home
In 2014, more than 106,000 French people benefited from HAD support. Affected by serious acute or chronic pathologies, they were hospitalized, in more than a quarter of the cases, in palliative care. But the HAD can also offer oncology support, monitoring of complex dressings (burns, ulcers or bedsores) or even perinatal care.
Home hospitalization is often confused with home nursing care, although it is a specific form of care, which is aimed at patients who are often seriously ill.
In fact, it is a real hospitalization: the health staff will set up, like a real hospital, a specifically dedicated room in the patient’s house. This assumes real upstream logistics, because the home must meet certain criteria. For example, the electrical system must be of high quality, so that medical equipment can function without problems.
Three doctors will then take turns at home: the hospital doctor, the treating doctor and finally a coordinating doctor, who takes over and monitors that the treatment protocol is respected. Paramedical professionals and nurses will also regularly visit the patient’s bedside (see box).
Skeptical hospital workers
Problem: ADH represents only 0.6% of all hospitalizations, a proportion that the government aims to double by 2018.
However, this schedule may not be tenable, if we are to believe the Court of Auditors, because the number of days spent in HAD throughout the territory is stagnating. After increasing by + 7.7% between 2011 and 2012, the rate of increase in the number of days rose to + 4.7% in 2013 and “only” + 1.9% in 2014.
There are several reasons for this slowdown. According to Sandra Gomez, medico-economic project manager of the FHF (1), the basic problem comes first from the ignorance of the actors of the health system about HAD.
“The added value of home hospitalization is not always well received by hospital doctors, especially for patients with severe acute illnesses. They therefore rarely refer to this type of care. However, a hospitalized patient can benefit from a HAD, which can allow him to leave conventional hospitalization more quickly, ”she underlines.
(1) French Hospital Federation
Affirm the role of the general practitioner
Moreover, hospital doctors are not the only skeptics. “More than a third of general practitioners are unaware that they can prescribe home hospitalization to their patients, without going through emergencies or prior hospitalization with accommodation”, underlines Eric Ginesy, national delegate of National Federation of HAD establishments.
A communication and awareness-raising effort is therefore required. To go in this direction, the Court of Auditors recommends in its report the realization of a larger number of socio-economic studies, in order to highlight the benefits of ADH, and to make it better known to physicians. .
Moreover, the very nature of home hospitalization requires close coordination between hospital doctors and treating doctors. However, this collaboration is not always optimal depending on the territory, and can lead to a deterioration in the quality of care.
Sandra Gomez therefore believes that it is necessary to re-mobilize general practitioners, so that they become benchmark players. “We have to motivate general practitioners. It is sometimes difficult to convince them to participate in the care protocol of a HAD because they do not see the usefulness of it, and because there are not enough of them in certain territories to free up the time to devote. to this support, ”she emphasizes. The Court of Auditors abounds in this sense, calling for a redefinition of the skills of each health professional.
Economic issues
Beyond these structural difficulties, it is on the financial level that HAD encounters the most problems. If the mode of care is often praised because it would cost less to the health insurance than conventional hospitalization, many hospital directors are reluctant to open a HAH service in their establishment. “Apart from palliative care, care in HAD is rarely profitable for the hospital,” explains Sandra Gomez.
However, each department benefits from at least one HAD structure. But the coverage of the territory remains very heterogeneous, because a large part of the structures are in Île de France, whereas in the mountainous regions, this support is almost non-existent.
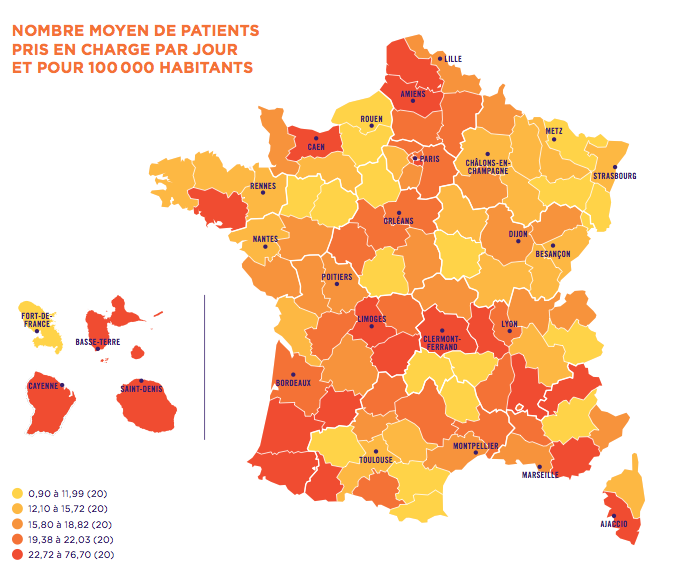
Source: National Federation of Home Hospitalization Establishments
“Given the population density and the isolation of certain municipalities, it is much more complicated to reach these patients. If we want to strengthen equal access to HAD, we have to review our pricing model to take these obstacles into account, ”observes Eric Genesy.
This is the solution also favored by the Court of Auditors, for whom the development of the HAD will not take place without a fundamental reflection on economic models.
The Ministry of Health has already launched a working group on the subject, in the hope that a clearer system will allow home hospitalization to develop, this time for good.
Prescribed by the general practitioner
The concept of home hospitalization was born in the United States in 1945. But France has also been a pioneer in the field since the 1950s. The first establishment to offer these services was created in 1957 in Paris. However, it was not until 1970 for the ADH to obtain legal recognition, and 2009 for it to be recognized as a full-fledged hospitalization, and no longer a simple alternative to traditional hospitalization.
A circular, published in 2000, specifies that this support is intended for individuals “suffering from serious, acute or chronic pathologies, who in the absence of such a service would be hospitalized in a health establishment”. In fact, a quarter of home hospitalizations today concern palliative care.
A patient alone cannot request a HAD. This must be prescribed by his attending physician, in the context of illness at home, or by a hospital physician, following conventional hospitalization.
The HAD service takes care of the administrative formalities with the Health Insurance and takes care of the fitting out of the room that will be used by the patient, at his home. The proper functioning of hospitalization must be based on close coordination between the hospital doctor, the coordinating doctor, the attending physician, and the paramedical and nursing staff.
To operate, the HAD establishment must be authorized by the State and certified by the Haute Autorité de santé. There are 270 in France, at least one per department.
Home hospitalization: The @Court of Audit tip the delays https://t.co/P1uumVTK4L #health #France pic.twitter.com/x0aLzXNhGc
– Pourquoidocteur (@Pourquoidocteur) January 22, 2016
.















