The WHO recalls the need to develop new drugs to enable doctors to fight against this STI.
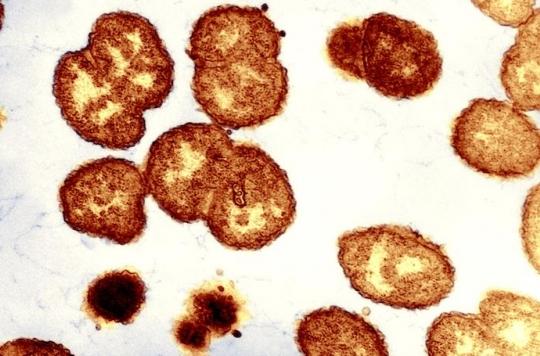
Commonly known as “hot piss” or “chill”, gonorrhea is one of the most common sexually transmitted infections (STIs). But it is also one of the most difficult to treat.
The World Health Organization (WHO) is concerned about the increase in antibiotic-resistant gonorrhea. It sounds the alarm on the occasion of the world congress on STIs and HIV organized from July 9 to 12 in Rio de Janeiro (Brazil).
“The bacterium responsible for gonorrhea is particularly intelligent,” explains Dr Teodora Wi, of the Department of Reproductive Health at the World Health Organization (WHO). Every time we use a new class of antibiotics to treat the infection, the bacteria evolve to resist it.”
Last resort antibiotic resistant
It is estimated that some 78 million people contract this infection every year worldwide, including 4.7 million in Europe. A very large number would be carriers of a bacterium resistant to old antibiotics. According to data from 77 countries, almost all of them register resistance to ciprofloxacin, azithromycin.
More worryingly, data collected between 2009 and 2014 indicate the emergence of resistance to drugs of last resort, broad-spectrum cephalosporins. This observation prompted the WHO to change its treatment recommendations in 2016.
But according to the WHO, the progression of antibiotic resistance could be even more important than expected, because the cases are mainly notified in high-income countries. They “represent only the tip of the iceberg because systems for diagnosing and reporting incurable infections are lacking in low-income countries where gonorrhea is actually more common,” Dr. Wi points out.
Better detect the disease
Currently, there is no rapid test to diagnose gonorrhea or a system capable of predicting which antibiotics will be effective against this infection. Result: caregivers treat infections blindly. Faced with a urethral or vaginal discharge, they sometimes wrongly prescribe antibiotics against gonorrhea when it is another infection. Inappropriate use that promotes the emergence of resistant strains.

To combat this phenomenon, the WHO is calling on laboratories to develop rapid and accurate tests that can be used at the point of care. New antibiotics are also eagerly awaited.
Currently, 3 drug candidates are in clinical trial. A relatively low number because industrialists do not get into the development of new molecules. “Treatments are only given for short periods of time and they become less effective as resistance develops, meaning there is a constant need to replenish the stock of new drugs,” describes the WHO. “In the longer term, we will need a vaccine to prevent gonorrhea,” adds Dr Marc Sprenger, director of WHO’s Antimicrobial Resistance Department.
In the meantime, prevention seems to be the best weapon to avoid new infections and to stem the spread of these multi-resistant bacterial strains. The correct and regular use of condoms is the simplest and most effective way. However, the decline in its use explains, in part, the rise of resistant gonorrhea.
An information and awareness-raising effort on this disease but also on other STIs is essential to encourage people to consult a doctor.
.