General practitioners have recently adopted a new guideline for the treatment of long-term pain. They will prescribe less heavy painkillers and help them cope better with the pain. Five questions about this new guideline.
1 What’s new in the area of pain?
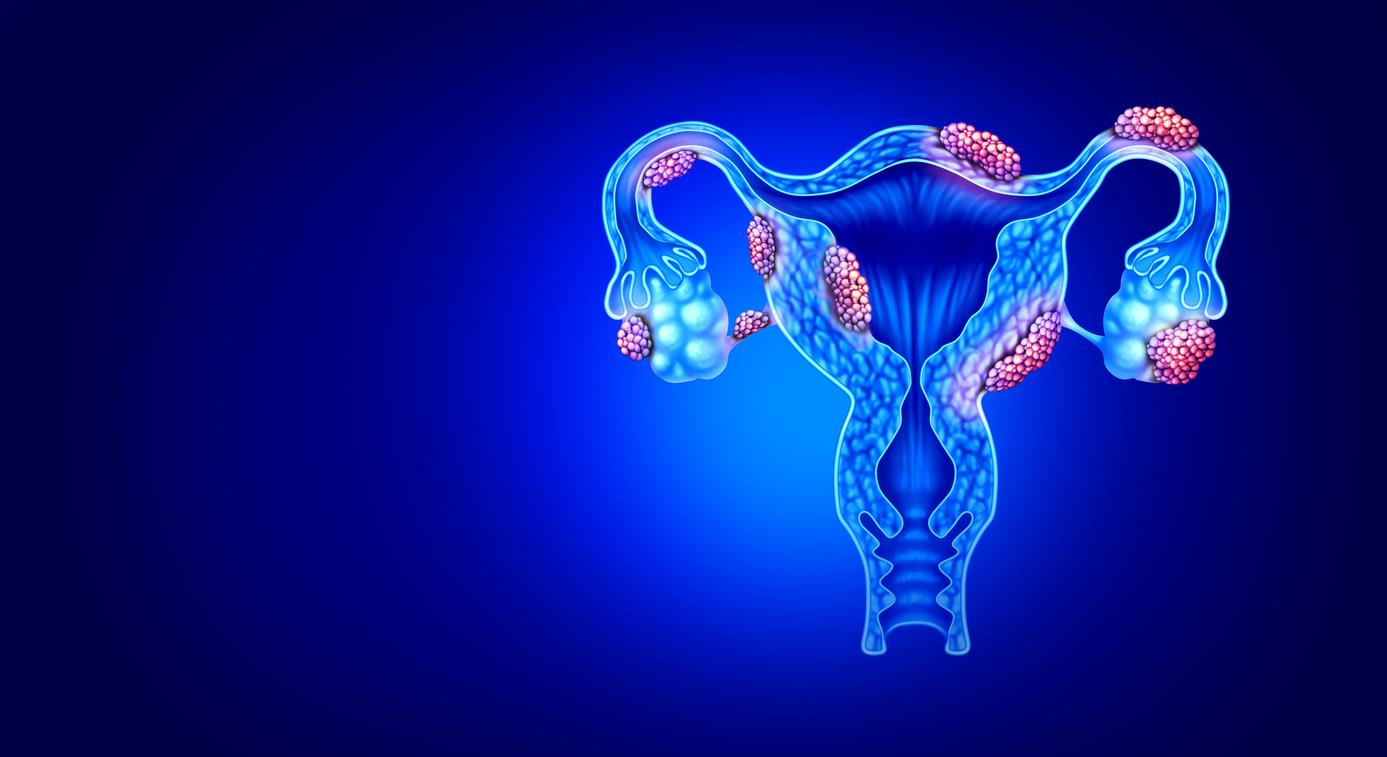
General practitioners are going to treat chronic, or long-term, pain differently. Chronic pain is severe pain that you keep walking around with, without a clear medical cause being found. For example, pain in the hip when walking, which has persisted for months. After an extensive investigation, no clear cause was found. Or think of pain due to a collapsed spine, osteoarthritis or a long-standing hernia. In these cases there is a physical cause, but you can feel much more pain than expected. The pain has gotten worse and lasts longer, while other people experience less pain in the long run.
2 How come you keep hurting for so long?
GPs call this phenomenon ‘sensitization’. This occurs when your nervous system continues to crank up the pain itself. Like a fire alarm that keeps going off, even if someone just walks by and there is no fire anywhere. ‘Sensitization’ has only been properly researched in recent years and is therefore now also included in the guideline. The consequences of the long-lasting pain: you worry, you get frustrated. A short walk already hurts, sitting for fifteen minutes already hurts. Some people lie flat on the bed, others overload their bodies by just going on and on. This behavior makes the pain worse.
3 What will the GP do about it?
With sensitization it makes no sense to look for the cause of the pain, because that usually does not explain the complaints (the fire of the fire alarm, there is none). GPs will prescribe fewer painkillers and refer fewer patients to specialists. On the contrary, they start looking for a different way to deal with the pain. For example, by looking for distractions. But also by seeking psychological help in coping with the pain. A physiotherapist can help you to exercise responsibly. A social worker can help with stress due to money or family problems. This allows the nervous system to relax and the pain is less. Sensitization decreases.
4 Is the pain ‘between the ears’?
Doeke Keizer promises in the GP & Science podcast that GPs will no longer come up with the discouraging ‘It’s between the ears’ or ‘Learn to live with it’. That overstimulated nervous system gives real pain signals, so the pain is definitely in the body. It’s not psychological, the pain is real. But the sensitization makes the pain worse, and you should try to reverse it. As mentioned, a psychologist can offer help with this. The trick is to calm down the nervous system and GPs want to pay more attention to this.
5 And the painkillers?
Painkillers do not help with chronic pain, as Thuisarts so clearly writes. The hypersensitivity of the nerves is not reduced by painkillers. The GP will therefore prescribe fewer painkillers and will be especially careful with morphine-like painkillers such as oxycodone. These drugs have many side effects and can even cause new pain, which you will not notice until you try to stop. Unnoticed, many people become accustomed to the heavy painkillers and the recipes are constantly repeated. You will therefore no longer receive the pills ‘if necessary, in case of pain’, but for a limited number of days.
Resources and more reading:
The NHG standard for pain was adjusted in November 2021. It can be read here, although it is quite difficult to understand because of the medical language. Fortunately there is also a more understandable explanation on the public-friendly website Thuisarts.nl. And for the more interested, a podcast has been recorded by the general practitioner magazine Huisarts & Wetenschap, it can be heard here. In this, GP Doeke Keizer, who obtained his doctorate in pain and involved in the guideline, explains what will change. The podcast is intended for general practitioners, but Doeke Keizer gives examples of patients with pain who explain a lot about the treatment of pain.