Researchers have used CRISPR-Cas9 technology known as “genetic scissors” to transform white fat cells into brown fat cells, which produce heat by burning calories.
- A genetic modification of immature white fat cells makes them similar to brown fat cells, which burn calories instead of storing them.
- Tested on mice, the genetic scissors technology allowed rodents to develop better insulin sensitivity and gain less weight.
Is gene therapy the future of the global fight against obesity and overweight?
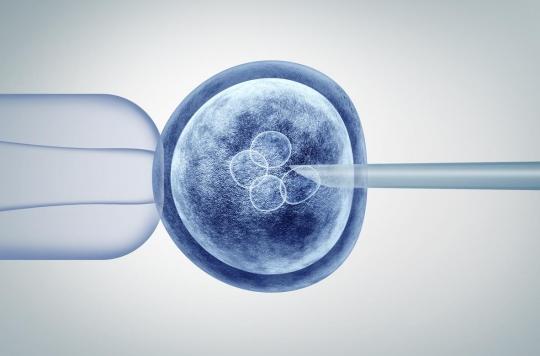
This is what a new study led by researchers attached to the Joslin Diabetes Center (United States) suggests. Published in the journal Science Translational Medicineshe shows the usefulness of the CRISPR-Cas9 technique, known as “genetic scissors”, to genetically transform white fat cells, which store calories, to make them similar to brown fat cells, which burn them to generate heat bodily.
“Brown fat cells burn energy instead of storing it like white fat cells do.explains Yu-Hua Tseng, a researcher in integrative physiology and metabolism at the Joslin Diabetes Center. By doing so, brown fat cells can reduce excessive blood glucose and lipid levels that are linked to metabolic diseases such as diabetes.” She points out, however, overweight or obese people tend to have less of this beneficial brown fat. Transformed brown fat cells, called HUMBLE (for “human brown-like”, human brown type) are however designed to overcome this problem.
Greater insulin sensitivity
The research team first created the HUMBLE cells from human white blood cells at an offspring stage, that is, not yet fully developed into their final form. They then used a variant of the CRISPR-Cas9 genome-editing system to boost the expression of a gene called UCP1, which triggers the development of white blood cell offspring into brown fat-like cells.
These HUMBLE cells were transplanted into mice lacking an immune system, which allowed them to grow. They then functioned like the mice’s own brown fat cells.
When fed a high-fat diet, mice fed HUMBLE Cells showed significantly greater insulin sensitivity and ability to clear blood glucose than mice in the control group. They also gained less weight.
Two options under consideration
For the researchers, these pre-clinical results are encouraging. They hope to soon be able to generate HUMBLE brown cells for individual patients. Such a procedure would thus consist of removing a minute amount of white blood cells from a patient, isolating the progenitor cells, modifying these cells to stimulate UCP1 expression, and then transplanting the resulting HUMBLE cells back to the patient.
However, says Dr. Tseng, this individualized approach could be complicated and costly. She is therefore working on alternatives. The first would be to use non-customized cells which would then be encapsulated by biomaterials that protect the cells from rejection by the patient’s immune system. The other option is gene therapies that directly express the UCP1 gene in the body’s white fat progenitor cells, so that these cells acquire HUMBLE-like properties.
“Using cell or gene therapies to treat obesity or type 2 diabetes used to be science fiction. Today, scientific advances, such as CRISPR gene-editing technologies, will help us to improve the metabolism, body weight, quality of life and general health of people suffering from obesity and diabetes”concludes Dr. Tseng.
.















