In Denmark, researchers have succeeded in creating artificial ovaries using a 3D printer to allow women whose fertility has been damaged by heavy treatment to have children.
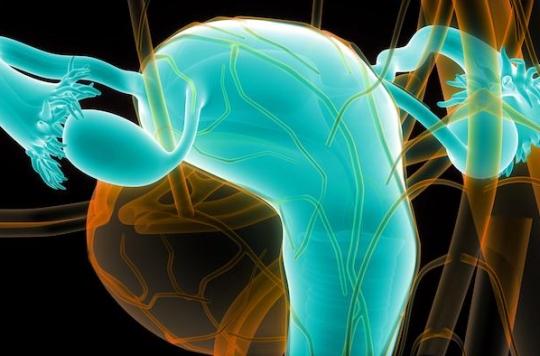
Researchers at Rigshospitalet Hospital in Copenhagen, Denmark, have developed artificial ovaries to allow women to have children after cancer treatment or other fertility-damaging therapies (early menopause, multiple sclerosis, beta-thalassemia …). Manufactured using a 3D printer, these ovaries would be able to keep human eggs alive for several weeks. A major breakthrough in the cure of infertility. In May 2017, American researchers explained in Nature Communications that “current technologies, including in vitro fertilization, hormonal treatments and ovarian transplants, do not provide long-term solutions and leave patients (especially young girls) without options”.
Currently, many patients freeze their ovarian tissue before undergoing their treatment, which they have reimplanted after recovery. “More than 30 children” were born after ovarian tissue freezing around the world according to figures from Human Reproduction Center (CRG). But if the practice is safe, it carries risks: in the event of heavy cancer, such as that of the ovaries or of leukemia for example, it is possible that cancer cells have invaded the ovarian tissues taken and that they are, of done, reimplanted into the body. The disease can therefore reappear.
958 follicles taken from 286 women
Based on this observation, researchers have developed artificial ovaries, a better alternative to infertility caused by certain heavy treatments, according to them. To do this, they stripped the ovarian tissue of all of its cells, including hidden cancer cells, leaving bare tissue made up largely of collagen. They then seeded it with hundreds of follicles, cells containing theoocyte who is released during theovulation.
A total of 958 follicles were collected from 286 women, with an average age of 28 years (16 to 43 years). The number of follicles collected from each woman ranged from 1 to 13 (mean 3.3 follicles / patient, median 3.0). The fluid was centrifuged and immediately stored at -80 ° C or, in some cases, instantly frozen in liquid nitrogen. Their study, published in the journal Frontiers in Endocrinology, was presented on Monday at the annual meeting of the European Society of Human Reproduction and Embryology in Barcelona.
“Exciting” results
Susanne Pors, one of the researchers, explained how the team managed to implant an artificial ovary containing 20 human follicles into a mouse and that a quarter of them survived for at least three weeks. During this time, blood vessels had started to develop around the ovary. If this study is a spectacular advance, Susanne Pors nevertheless specifies “that it will take many years before the experiment is carried out on a woman. Five to 10 years of work are necessary for the artificial ovaries to be ready”.
Nick Macklon, medical director at the London Women’s Clinic, told The Guardian that although the risk of contracting cancer again from frozen ovarian tissue was low, the risk was real. “We cannot do this because of this concern in some cases,” he said, praising the “exciting” results of this promising study. Stuart Lavery, consulting gynecologist at Hammersmith Hospital, added: “It will be very reassuring if this work comes to fruition that patients can receive the transplant knowing that there is no risk of reintroducing the cancer.” Doctors therefore seem unanimous as to the innovative and revolutionary nature of this advance.

.















