In a new press release, the High Authority for Health (HAS) recommends systematic screening for chlamydiosis in all young women.
Chlamydia may be one of the most common sexually transmitted infections (STIs) in young, sexually active women, but it remains relatively unknown. Caused by a bacterium (Chlamydia trachomatis), it is now the subject of particular attention from the High Authority for Health (HAS). In a statement made public on Tuesday, October 27, the organization recommends systematic screening for young women aged 15 to 25 who are sexually active.
An asymptomatic sexually transmitted infection
Because there is an urgent need to stop the progression of chlamydia, estimates the HAS. Affecting nearly a million people in France, this STI can be treated with antibiotics when detected. However, chlamydia is, in the majority of cases, asymptomatic: between 60% and 70% of women infected with the bacteria do not feel any symptoms and are therefore unaware that they have contracted it. “This promotes the occurrence of complications and the transmission of the bacteria within the population”, explains the High Authority for Health.
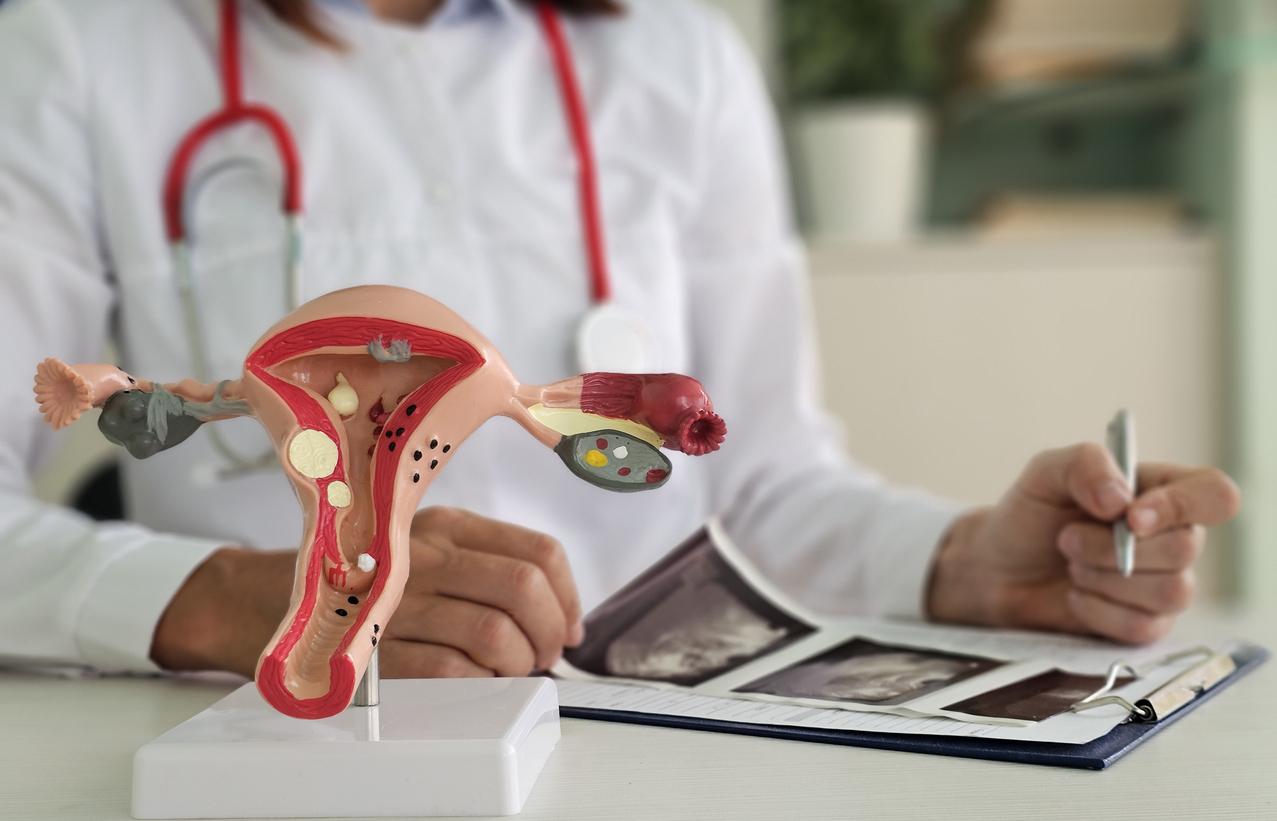
This makes her particularly fearsome. If not treated in time, the infection can cause severe complications in young women, such as “pelvic inflammatory disease, salpingia, ectopic pregnancy or tubal infertility (blocked tubes)”, lists the HAS. Some strains of the disease also cause trachoma, an eye infection that can cause blindness. Chlamydiosis infection remains the main cause of blindness in underprivileged countries.
“As much in men there can be obvious symptoms as they often develop urethritis, which is irritation of the urinary tract with tingling while urinating and discharge. But in women it is much more complicated, explain to Figaro Dr. Jean-Marc Bohbot, infectious disease specialist, medical director at the Alfred Fournier Institute in Paris.
Systematic screening to limit the spread of infection
According to the High Authority for Health, screening will not only “reduce the risk of long-term complications in women”, but also “limit the spread of infection within the population, thanks to early treatment”. . This annual screening could be repeated every three to six months after treatment in the event of a positive result, recommends the HAS. The organization wants to make it systematic for sexually active women aged 15 to 25, including pregnant women.
“Opportunistic” screening could also be offered to men regardless of their age, as well as to “pregnant women consulting for an abortion without age limit” and to women over 25 who present risk factors. These factors are numerous: multi-partnership, recent change of partner, man who has had homosexual sexual relations, prostitution, individuals or partners diagnosed with another STI, after rape, etc.
The High Authority for Health recommends that screening should above all be carried out by general practitioners, gynecologists and midwives. It can also be carried out by self-sampling, vaginal for women, urinary for men, and offered in all screening locations. On the other hand, estimates the HAS, the rapid diagnostic tests (RDTs) “are not sufficiently effective today in the detection” of chlamydia.
The effectiveness of opportunistic screening questioned
Although recommended by the High Authority for Health and the health authorities of several countries, opportunistic screening for chlamydia is the subject these days of a study which calls into question its effectiveness. In an article published on October 20 in the journal The Lancet, researchers from the University of Melbourne say they studied the effects of opportunistic chlamydia screening in primary care on the estimated prevalence of STIs in Australians aged 16-29.
Between 2010 and 2015 and over a period of 3 to 1 year, 93,828 young adults in 63 clinics benefited from opportunistic screening for chlamydia twice: before randomization (survey 1) and at the end of the study (survey 2). A further 86,527 were followed in control clinics that did not practice STI prevention or opportunistic screening.
At the end of their research, the scientists found that the estimated prevalence of chlamydia decreased from 5% to 0% at survey 1, and to 3-4% at survey 2 in the groups where screening opportunist was realized. In the control groups, the prevalence declined to 4-6% at survey 1 and 3-4% at survey 2. “These results, together with the evidence on the feasibility of sustained use of opportunistic testing in the primary care setting, indicate that it may not be possible to significantly reduce the prevalence of chlamydia,” the study authors write.

.