Still 40% of women do not participate in organized cervical cancer screening in place. For the French Society of Colposcopy and Cervico-Vaginal Pathology (SFCPCV), self-sampling could convince them to get screened.

- The SFCPCV notes that some doctors do co-testing when screening for cervical cancer. However, this does not improve the effectiveness of screening.
- Despite the campaigns and invitations sent, 40% of women do not get screened for cervical cancer.
- For the SFCPCV, self-sampling could make it possible to reach these patients who do not have access to a doctor or do not want to go to consultations as well as those who do not respond to screening invitations.
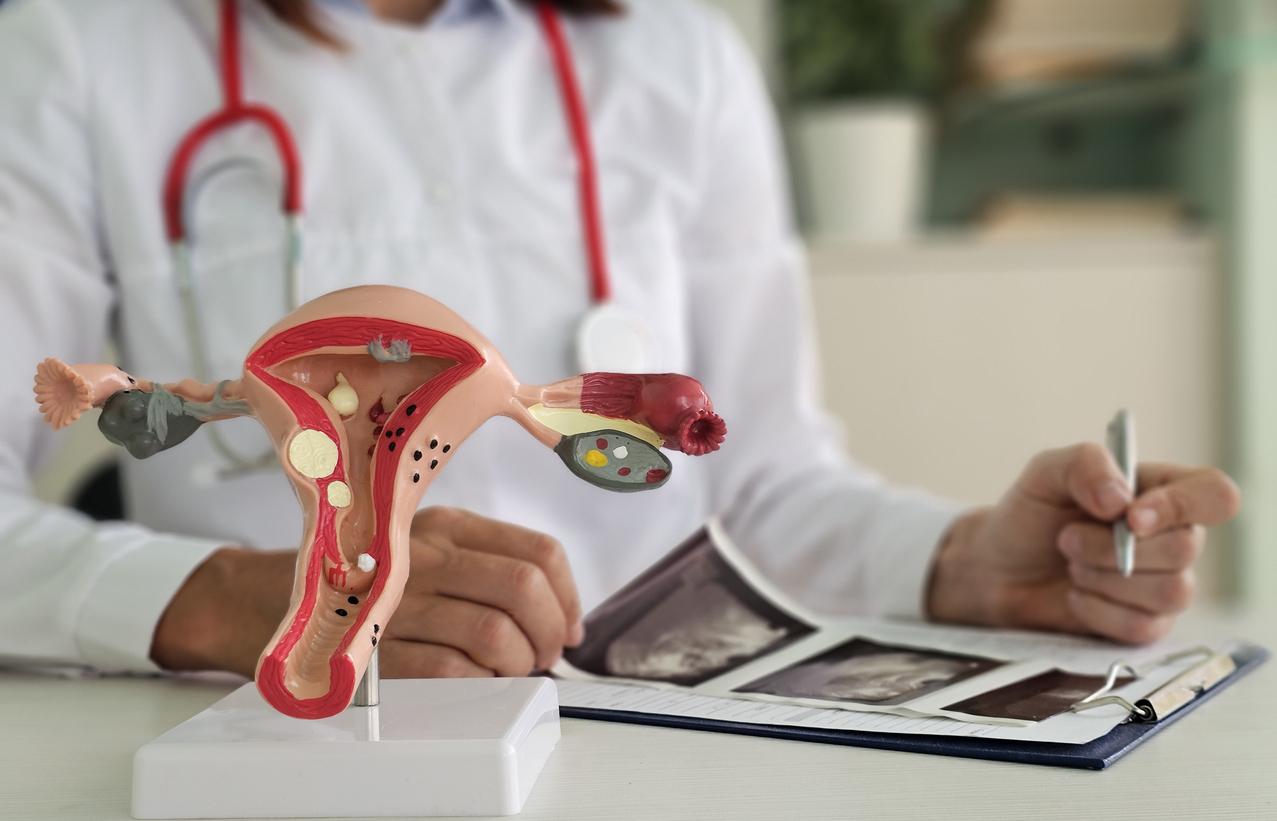
There are 3,000 new cases of cervical cancer and 1,000 deaths linked to this disease per year in France. One of the tools to fight against this type of pathology is organized screening. But for the French Society of Colposcopy and Cervico-Vaginal Pathology (SFCPCV) which held its 47th National Congress, improvements must be made to reduce the incidence of cervical cancer and convince more women to have screen.
Organized cervical cancer screening: beware of co-testing
Cervical cancer screening is offered to all women aged 25 to 65, unless otherwise directed by a doctor. Since 2020, it is recommended that patients under the age of 30 be screened through a cytological examination, while the HPV-HR test is recommended for those aged 30 and over.
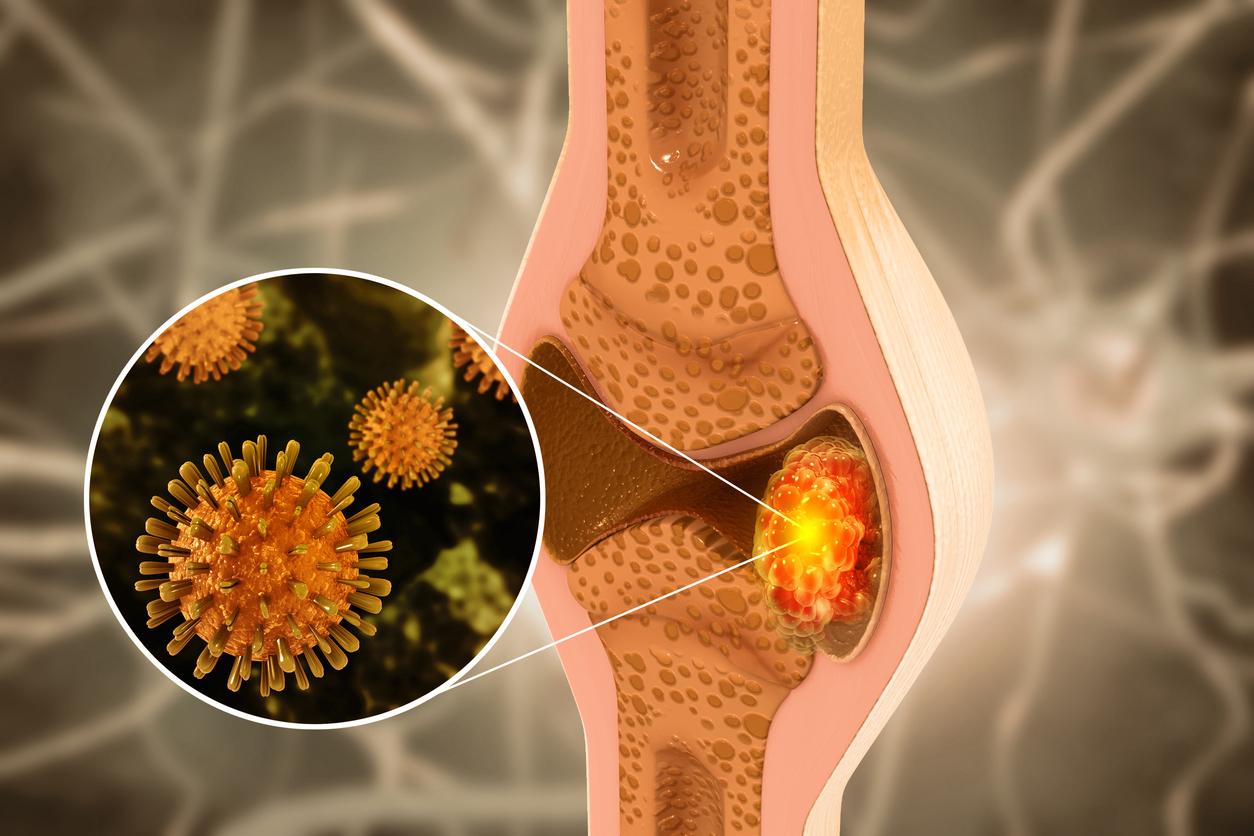
Unlike cytology which studies the appearance of the cells collected during the smear, the HPV-HR test looks for the presence of the high-risk HPV virus, a risk factor for cancer.
“We have thus changed the way in which doctors have worked for 40 years since it was cytology which was used for all women after the Second World War”explains Dr. Christine Bergeron, SFCPCV anatomopathologist.
And although this cervical cancer screening has been well adopted by all health professionals, a shortcoming has emerged. “Despite the recommendations, doctors can do the tests they want. And some professionals have done what is called co-testing. That is to say, for their patients between 30 and 65 years old, they carried out the recommended HPV-HR test, but also the cytological examination”, indicates the expert. The problem with this method? “Studies have shown that doing both tests is worse than doing only HPV. This can give positive cytologies while the HPV-HR test is negative. These unnecessary tests worry the woman and lead to unnecessary colposcopies, and did not in any way improve the effectiveness of screening.”
Administrative management of the transfer of patient analyzes to screening centers, different software between regions and departments, etc. Several obstacles have slowed down the effectiveness of invitations to organized cervical screening in recent years. “The rate of organized screening increases gradually every year, but it remains low. Today, 13% of women respond to the invitation compared to 10% in 2018”adds the expert. “We hope that in the years to come, we will be able to reach the 40% of women who do not get screened in one way or another.”
“Covering 60% of the population we know how to do, it’s relatively easy. On the other hand, each percentage gained in coverage requires efforts which become exponential”warns Professor Xavier Carcopino, president of the SFCPCV.
HPV: self-sampling to attract women who do not undergo organized screening
For the professional body, one of the solutions to reach these women who do not go for consultation despite invitations to organized cervical cancer screening could be self-sampling.
“It is the possibility for a woman to take the sample herself which will be used for her HPV screening. This can come in different forms, but the most common is a vaginal swab. The equivalent of a small cotton ball rod that the patient will insert herself into the vagina. It is then placed in a transport bottle and then sent to the laboratory”, explains Professor Xavier Carcopino.
This method has the advantage of being accessible to women who do not have access to a doctor or do not want to go to consultations as well as those who do not respond to screening invitations.
“This test has been highlighted since last year, because the INCA and the HAS highlighted the possibility of using it. They recognized its value, based on numerous scientific studies which clearly show that this sample works. Above all, it allows us to increase screening, because it reaches patients who would not be screened with health professionals.”
However, the gynecologist warns: “this test will not allow everything”. Although it may appeal to women who do not normally undergo screening, it does not allow cytology to be carried out. “That is to say, there is no cell sampling with the latter. It only collects samples of vaginal secretions and thus only determines the presence or absence of papillomavirus”adds the expert.
Another downside: women whose self-sampling comes back positive are still obliged to consult for cytology, then possibly a colposcopy. Additionally, it reduces interaction with the doctor – and by domino effect – access to information about cervical cancer as well as other health topics like contraception, HIV, STDs, female cancers, gynecological follow-up…
“For the moment, this self-test has not yet been sent to women. But what is looming, and what the texts validated by the INCA and the HAS propose, is the sending of self-tests in the coming months to patients who did not respond to their first invitation. This has been recorded. But a decree must be published in the Official Journal for this to be launched.”specifies Professor Xavier Carcopino.
“Self-debit works, but it will not reach 100% of the population, recognizes the president of the SFCPCV. On the other hand, this will allow us to gain 10%. But 10%, that’s hundreds of patients screened with cancers avoided.”