At the Society of Interventional Radiology’s latest meeting held virtually on June 13, researchers presented a promising new non-surgical treatment to decrease errant blood flow in the shoulder of patients with capsulitis.

- Adhesive shoulder capsulitis (ERC) or “frozen shoulder” is an inflammation of the shoulder joint envelope.
- It affects 2 to 5% of the general population.
- Researchers have presented a promising new non-surgical treatment to decrease errant blood flow in patients’ shoulder.
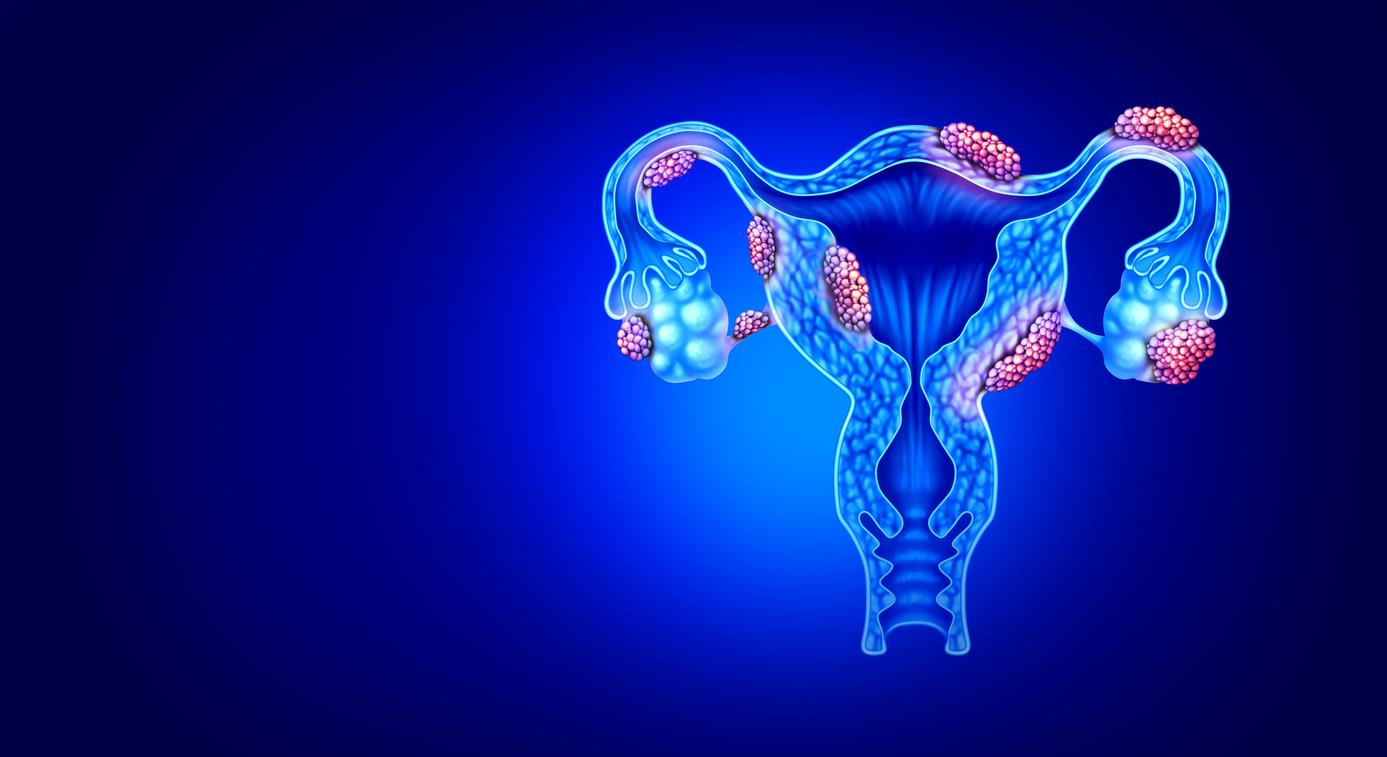
The adhesive capsulitis of the shoulder (ERC), or “frozen shoulder”, is an inflammation of the covering of the shoulder joint (called the joint capsule). It is manifested by a sudden acute pain to which is added an overall rigidity of the shoulder. These symptoms are most often treated with physiotherapy or painkillers and take between one to three years to resolve. During the 2020 scientific meeting of the Society of interventional radiology held virtually on June 13, researchers presented a new non-surgical treatment to decrease errant blood flow in patients’ shoulder. This promising technique would quickly reduce pain and improve patient mobility.
In an FDA-approved Phase II clinical trial of arterial shoulder embolization (AES), interventional radiologists inserted a catheter through a pinhole-sized incision in the wrist of patients. This one had been used to feed microsphere particles into no less than six arteries in the shoulder to reduce inflammation. Each patient’s pain, disability, and blood flow in the shoulder were measured before and after treatment using three scales, in addition to MRI imaging to visualize the shoulder joint.
“Patients with a frozen shoulder are essentially told to hold off until their symptoms improve, but given the significant pain and decreased function that many experience, we set out to determine whether this pattern treatment of embolization, already used in other areas of the body, could provide immediate and lasting relief”explains Sandeep Bagla, lead author of the study.
“We were surprised by the profound and dramatic improvement in pain”
The treatment was completed in 16 patients. Minor adverse effects such as temporary skin discoloration were reported in nine subjects. A month later, the researchers followed the evolution of 11 patients in whom the pain had decreased significantly after BEA. Physical function improved in all, and further progress was reported at the three-month follow-up.
“We are early in the study of this treatment, but we are inspired by its effectiveness in reducing pain and range of motion in patients’ shoulderswelcomes Sandeep Bagla. We were surprised by the profound and dramatic improvement in patients’ pain and use of their shoulder.”
However, this treatment is still under study. Moreover, the experiment has some limitations, such as the small sample size or the absence of a control arm. In order to go further, it will be extended to other patients in 2020. While waiting to learn more, conservative therapies must continue to be considered as a priority, conclude the researchers.
Many risk factors
Adhesive shoulder capsulitis affects 2-5% of the general population. It is sometimes due to trauma to the shoulder or to surgery or radiotherapy axillary or supraclavicular. It can also be the consequence of a myocardial infarction, a neurological disease (stroke, Parkinson) or diseases metabolic (diabetes, thyroid dysfunction) or pulmonary. It also happens that the long-term intake of barbiturates or certain anti-tuberculosis treatments (isoniazid and ethambutol). Finally, an anxious ground is sometimes put forward as a risk factor but this has not yet been scientifically demonstrated. To diagnose capsulitis, the most effective examination is MRI.
.