According to a new American study, the killer fungus Candida auris, more and more widespread throughout the world, would have developed with global warming.
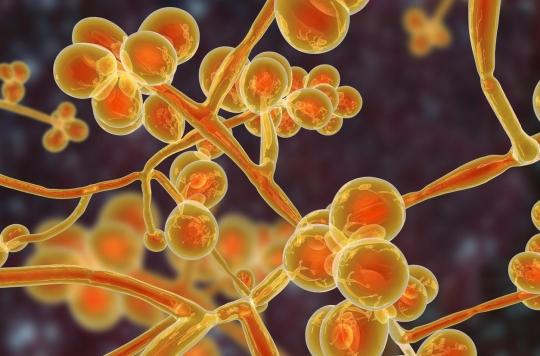
candida auris. This is an unpleasant-sounding name that comes up more and more in the press. A few months ago, the New York Times published a dossier on this killer fungus that has become resistant to drugs and is increasingly observed in Southeast Asia, India, South Africa, the United States and Europe. According to the latest data, it seems that more than a third of patients who contract it die from it. Today, a study published in the scientific journal mBio tells us more about the origins of this infection. The latter would have developed with global warming.
It was in 2009 that the first case of candida auris is reported. Doctors identify a fungus in the ear canal of a Japanese man. Since then, the infection has been spotted in hospitals all over the world without anyone really understanding why. “Since that first isolation in Japan, C.auris has been implicated in candidaemia and invasive infections associated with high morbidity and mortality”, detail mycologists for the French Society of Hospital Hygiene in an article published in May.
Today,”the biggest mystery yet to be understood is how the same species of fungus grows on three continents. at the same time. They are different societies and populations, but they have something in common, the world is getting warmer,” says Dr Arturo Casadevall, director of the department of microbiology and immunology at Johns Hopkins Bloomberg School of Public Health in the United States. and lead author of the new study.
Rising mercury should help new germs infect us
Arturo Casadevall and his colleagues therefore decided to study fungi close to candida auris. They found that the majority grew well in ambient air but could not survive human body heat. Thus, the one causing the deadly fungal infections would have adapted to higher temperatures.
Rising mercury caused by global warming will eventually push new germs into the ‘thermal restriction zone’, an area so hot it usually keeps most species out, scientists say in our body. Also, without effective defences, new resistant fungi will be able to infect us much more easily.
Moreover, according to US Centers for Disease Control and Prevention, most known resistant strains have at least one of the three drug classes used to treat fungal infections. According to their observations, more than a third would be resistant to two out of three treatments.
An infection that occurs in immunocompromised people
To date, infections due to candida auris have been spotted in more than thirty countries. However, they are difficult to detect since they occur in people who have already been treated for another infection and whose immune system is already weakened.
“The germ emerges in patients who have received antibiotics, who are very immunocompromised (whose immune system is weakened, editor’s note), who are notably in intensive care, hematology or transplant departments”, specifies Professor Didier Lepelletier , head of the hospital bacteriology-hygiene department of the Nantes university hospital center, quoted by Release. Patients often suffer from fever and chills that do not respond to standard antibiotic treatment.
This superbug is so contagious that staff at Brooklyn Hospital (New York, USA) have already had to disinfect the room of an affected patient with “special cleaning equipment and had to remove part of the ceiling and of the ground”. In 2016, in London, the Royal Brompton hospital even had to be closed for almost two weeks for decontamination.
.