About 25,000 Dutch people get a new hip every year. But which artificial hip is the most suitable? And … is the hip swing still allowed if you dance the tango again?
1. How do hip complaints arise?
The ends of the bones of a healthy hip joint fit together like a sphere in a bowl. They are covered with soft cartilage, so they can move smoothly and painlessly past each other. With age, the cartilage wears down. In time, it may even disappear completely. The bone ends then become rough and rub against each other. This causes pain when moving and stiffness. This type of wear is called osteoarthritis. 20 percent of all over 55s suffer from some form of arthrosis. That is even 90 percent of all people over 65. In addition to osteoarthritis, a (congenital) disease or a broken bone can also lead to hip complaints.
2. Do we ourselves influence the extent to which our hip joint wears?
Yes. Under heavy loads, the joint wears out faster. People who are overweight more often have a worn out hip and intensive athletes also demand a lot from their joints. That does not mean that all movement is bad, on the contrary. Exercising in moderation is good to keep the joints flexible. It massages the cartilage, as it were, and stimulates the absorption of nutrients. Even if a hip joint is already worn out, it is good to keep moving. Even if it hurts. If you move less, the hip will become stiffer.
3. When should a worn hip joint be replaced?
When the pain gets so bad that you can’t do what you want. Physiotherapy or medicines can ease the pain, but osteoarthritis cannot (yet) be cured. When the pain complaints become so severe that they make a normal life impossible, a hip prosthesis is the solution. In that case, the worn parts of the hip are (partially) removed and replaced by an artificial joint.
4. Is there a minimum or maximum age for a hip replacement?
New. When a patient receives an artificial hip relatively young (before the age of 50), there is a good chance that it will have to be replaced once or twice at a later age.
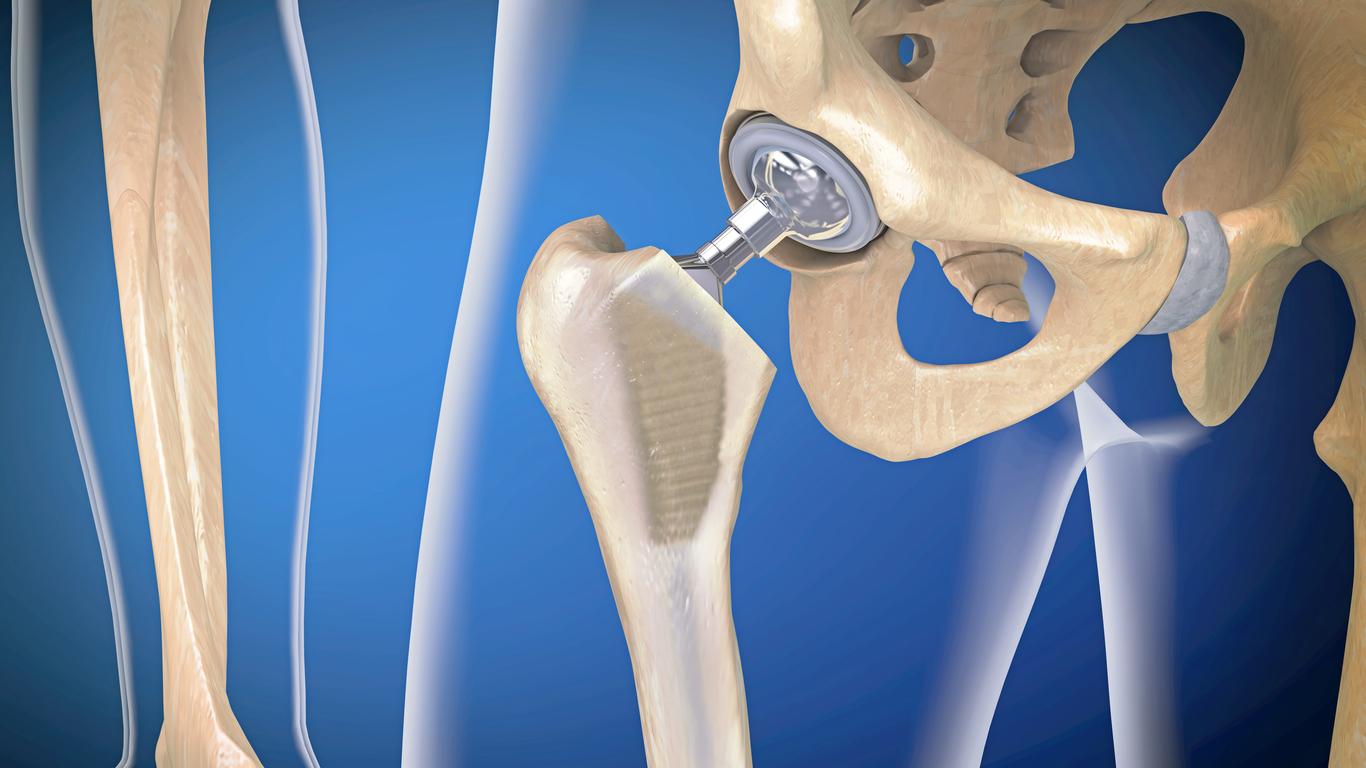
5. How does a hip replacement work?
Thanks to modern techniques, damaged parts of a hip joint can be replaced, preserving as much of the bone as possible. In a primary hip prosthesis, the damaged parts of the hip joint are replaced by a prosthesis consisting of a stem with a head and a hip socket. The hip stem is placed in the femur and the hip socket in the pelvis. A ball-shaped head is attached to the hip stem that can move in the hip socket. A modern hip joint lasts longer than ten years on average. after that time, revision surgery may be required. It is possible to partially replace the hip prosthesis during revision surgery.
6. Men and women are built differently. Do they also get different hip replacements?
Various prostheses are used in the Netherlands. Which prosthesis is suitable for which patient depends, among other things, on the condition and the physique. There are no specific prostheses for men or women.
7. Does a hip replacement always fit?
They come in many shapes and sizes and are therefore suitable for almost everyone. In very exceptional cases, for example in the case of a bone tumor in the hip, it may be necessary to make a custom prosthesis.
8. What material is a hip prosthesis made of?
Depending on the shape and nature of the prosthesis, it contains different materials: plastic, ceramic or metal (titanium/chrome cobalt).
9. Does the prosthesis grow into the bone by itself?
Half of the people do. In the other half the quality of the bone is insufficient or the prosthesis cannot be clamped. The prosthesis is then secured with bone cement during the procedure. The patient does not notice any difference: the freedom of movement is the same in both cases.
10. Which hip replacement is the best?
There is no ‘best hip replacement’. Which prosthesis is most suitable depends on, for example, age, general condition and lifestyle of the patient. The proven results of the prosthesis and the experience and personal preference of the doctor also play a role in the choice.
11. How long does the recording take?
Often, after an average of four or five days, the patient can get in and out of bed, walk, climb stairs and get into the car. Usually they can go home. Rapid Recovery is used in some clinics. The principle of this is that rapid mobilization leads to a better and faster recovery.
12. What does the rehabilitation process in the hospital look like?
Rehabilitation begins the day of surgery or the day after, depending on whether Rapid Recovery is used. A physiotherapist will teach you exercises in and out of bed. You may put a little more load on your hip prosthesis; first you walk with a walker, then with crutches and then gradually without support. Climbing stairs is also practiced. You should expect to leave the hospital on crutches.
13. What is the Surgery Success Rate?
Research shows that almost all hip prostheses work well. About 98 percent of patients can move better with the new hip and usually the pain is completely gone.
14. What are the possible dangers?
In up to 5 percent of patients with a total prosthesis, the hip may dislocate when, for example, they squat or bend deeply. In most cases, no further surgery is required to correct this problem. By pulling and simultaneously turning the leg, the orthopedic surgeon tries to get the femoral head back into the socket; the patient will then first be given muscle relaxant medication.
In 1 to 1.5 percent of cases, an infection develops in the new hip joint. That percentage is no higher than after comparable operations.
15. How does the rehabilitation process work at home?
You will need help for the first few weeks. Hire someone to run errands and help you with household chores. Do the exercises instructed by your physical therapist and orthopedic surgeon. You will eventually be able to fully use your hip joint again after about six to twelve weeks. Alternate rest and activities. In principle, climbing stairs is not a problem, although it is sometimes difficult in the first weeks after the operation.
16. Is physiotherapy always necessary after surgery?
Yes. It is advisable to continue exercising after discharge from the hospital, at home and with a physiotherapist. Guidance from a physiotherapist is necessary to learn to walk properly again without crutches. You will need physical therapy twice a week on average for two to three months. As soon as you know when you will be operated on, contact the physiotherapist immediately to schedule an appointment for after hospitalization.
17. When can I drive again?
To accelerate, shift and brake you need good control of your leg. You can usually drive again six weeks after the operation. This also applies to flying, due to the increased thrombosis risk after surgery. Stretch your legs in between on a flight of longer than two hours.
18. How can I best protect my artificial hip?
By some simple precautions.
- Prevent infection: If you get an infection anywhere in your body, for example an infection on the skin, toes, bladder, lungs, throat or teeth, it can get into the bloodstream and spread to your hip. Therefore inform your doctor if you suspect that you have an infection.
- Inform the surgeon for any other surgery: If you have another surgery in the future, tell the surgeon that you have a hip replacement, because of a possible risk of infection. Even if it concerns a minor operation such as dental procedures.
- Prevent overweight: with the correct body weight, the pressure on the new hip is not too high. And keep moving!
- Other points to watch out for: never bend more than 90 degrees; when sitting, keep knees lower than hips; keep your legs 15 centimeters apart when sitting or lying down; use a raised toilet and a seat in the bath if possible; wear comfortable shoes, without high heels.
19. What about sports?
Sports such as football and running can shorten the life of the prosthesis. It is therefore better not to practice this with a hip prosthesis. You can dance the tango, but in moderation. Skating, skiing, cycling, swimming, golf, tennis, fitness and walking are generally not harmful to the prosthesis. Always consult your doctor. If necessary, he can refer you to a sports physiotherapist.
Sources):
- Plus Magazine