We often hear about the phenomenon but without knowing what it is really about. What is a coma? Why do we fall into this state of altered consciousness? What is the difference with brain death?

- The artificial coma is a controlled coma caused by sedative drugs to be able to treat the patient, for example in the event of cerebral edema. The idea is to put the brain to rest, to be able to process it better. It’s an artificial coma, so better controlled.
- Alcoholic coma is caused by excessive alcohol consumption. It usually only lasts a few hours, but it can leave neurological scars. There are also other types of comas such as diabetic coma or hydraulic coma.
For most of us, including the medical world, the coma remains mysterious. People can dive there for a few hours or several weeks or even years. But what does it mean, exactly, to be in a coma?
What happens when you fall into a coma
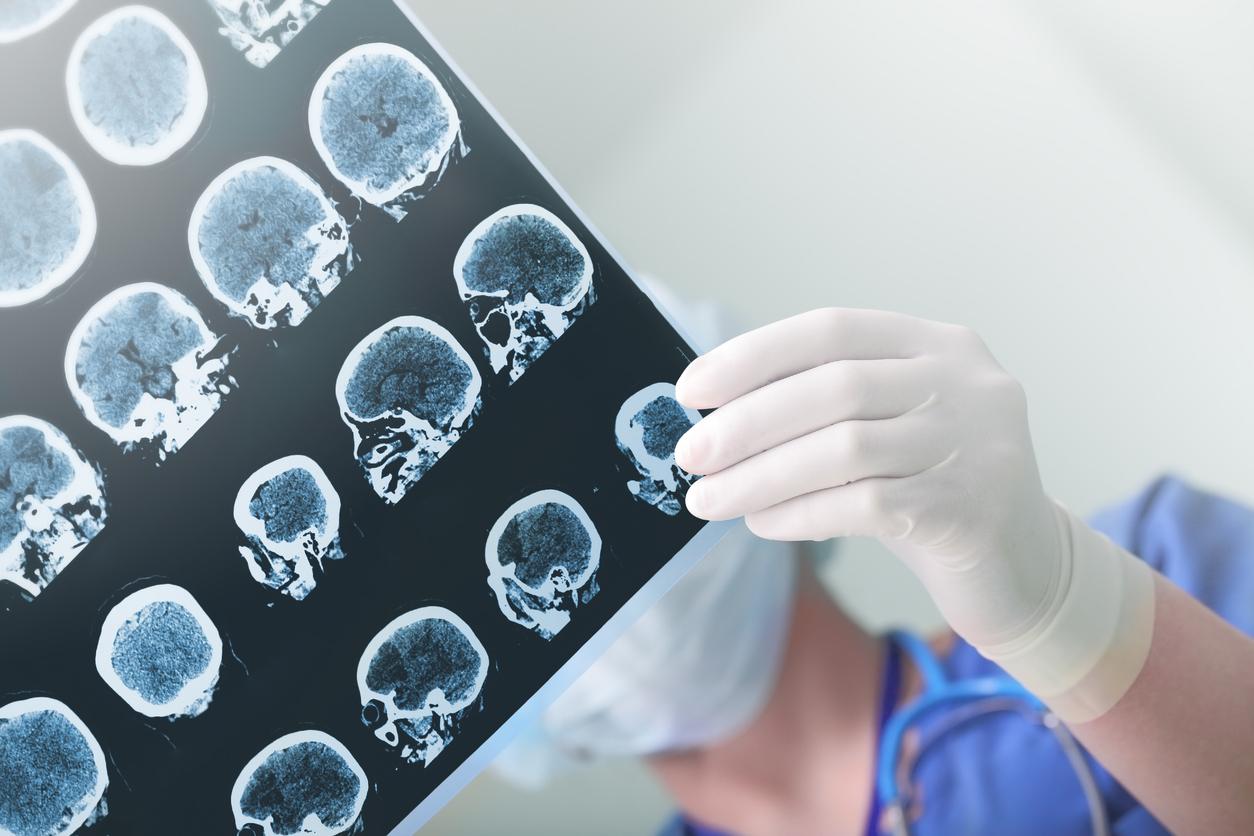
Coma can result from head trauma, stroke, brain tumour, meningitis, alcohol or carbon monoxide poisoning… Traumatic comas (more than 50% of cases) are distinguished from non-traumatic comas. traumatic, that is to say which are not generated by a shock to the patient. How does it work concretely? Due to a lesion, a lack of blood or oxygen supply, or an inflammation that will compress the brain, the brainstem – essential for transmitting information and orders from the brain to the organs – will start to malfunction, with serious consequences. There is in particular in this brain stem an area called reticular formation which is involved in vital functions such as sleep-wake cycles, control of motor functions (such as walking) or cognitive functions (vigilance, attention). When this area is injured, the person finds himself literally cut off from the outside world: in a coma.
The longer the coma, the more brain damage
“Coma is the most severe form of impaired consciousness”, according to the National Institute of Health and Medical Research. Coma is not brain death, defined by the total and definitive absence of brain activity, and therefore of cardiovascular and respiratory functions: the patient lives only thanks to resuscitation assistance machines, and that is irreversible. In a coma, the patient is very much alive, his functions are preserved and his brain is still irrigated with blood. But the person is unconscious, eyes closed, unable to react to external stimuli (pain, light, noise…) or to be awakened from his “sleep”. She can wake up, but the longer she is in a coma, the higher the risk of brain damage.
Other states of altered consciousness
There are several stages of coma. Doctors classify depth based on the three criteria of the Glascow scale: eye opening (spontaneous or triggered), motor response and verbal response. By adding the results, they determine the level of coma between 3 (deep coma) and 15 (the person is perfectly conscious), knowing that 8 is an official “coma”. Although the classification into four stages, long used by doctors, is now obsolete, this gives an idea of the different states of consciousness: stage 1 or coma called vigil (the patient feels pain and pronounces a few understandable sentences), coma mild (impossible to communicate, no neurovegetative disorder), carus coma (deep coma, absence of verbal and motor responses, neurovegetative disorder) and stage 4 or overcome coma (so-called brain death).
The coma is “generally a transient state” which lasts only a few days, “at most a few weeks”, recalls Inserm. But the return to consciousness can also be slow and gradual, passing through other states of altered consciousness, such as the vegetative state in which the patient opens his eyes but is not conscious. They can even stay there for years, halfway between coma and consciousness.