One in four patients in a coma or vegetative state due to brain damage may actually have some level of consciousness, according to a new study led by Mass General Brigham.
- 1 in 4 patients with severe brain injuries who appeared unconscious were secretly responding to instructions, a new study finds.
- This little-known phenomenon is called motor cognitive dissociation.
- For researchers, it is therefore essential to carry out further work on this disorder and improve communication methods such as brain-computer interfaces.
Some patients in a coma or in a vegetative state due to severe brain damage would respond “secretly” to the instructions given to them.
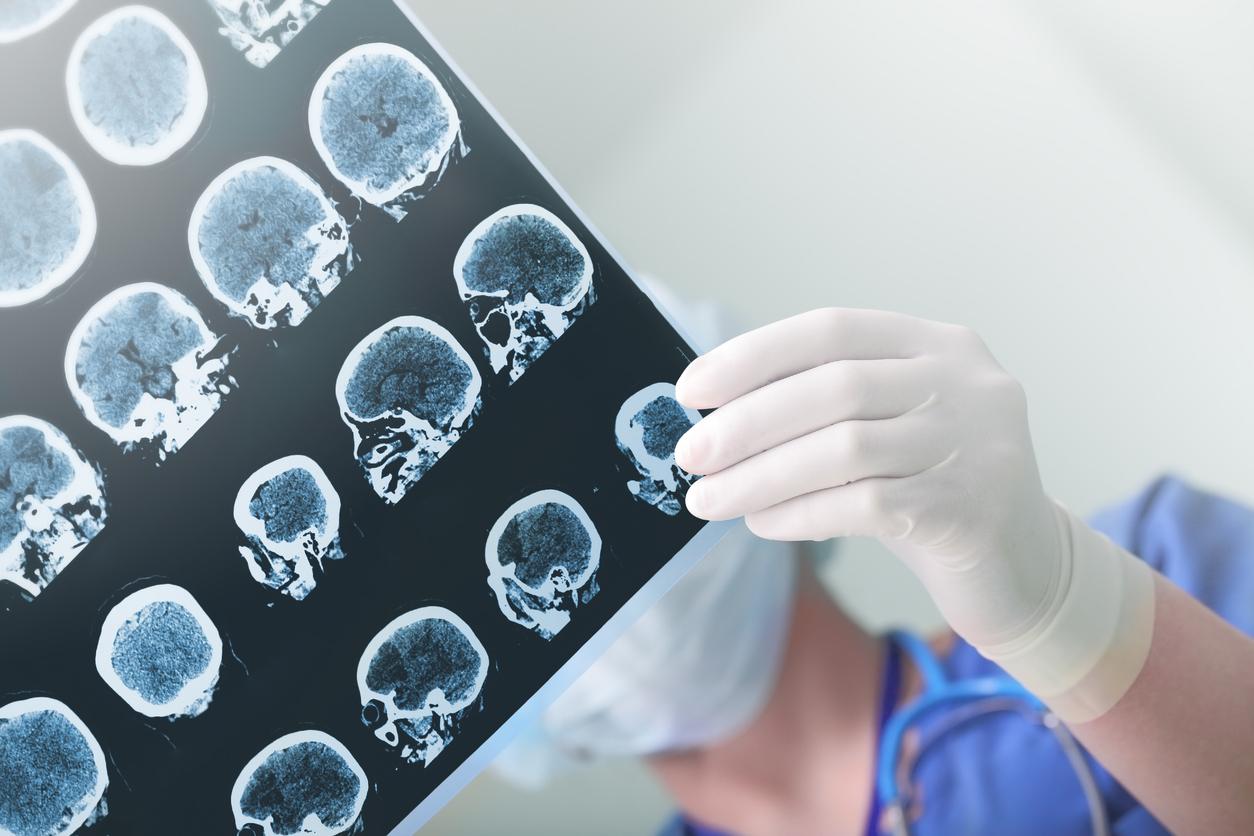
Researchers at Mass General Brigham have noticed that brain scans have detected signs of consciousness in some patients with severe brain injuries who show no physical response to their surroundings.
Their study was published in the journal New England Journal of MedicineAugust 15, 2024.
Brain injury and coma: consciousness detected in 25% of patients
To further assess the incidence of motor cognitive dissociation (a disturbance of consciousness following brain injury in which the patient is no longer responsive but has cognitive abilities), the researchers followed 241 participants with severe brain injuries who did not respond to a simple instruction. They had them undergo a functional MRI (fMRI), an electroencephalogram (EEG), or both. During these scans, the patients heard instructions such as: “imagine opening and closing your hand”. They were followed 15 to 30 seconds later by “stop imagining opening and closing your hand.”
The tests revealed that 25% of them had brain responses suggesting that they were “mentally” following this instruction repeatedly and for several minutes, even though the professionals did not perceive any movement. This figure is higher than the assessment given in the first study on motor cognitive dissociation. It had estimated that this phenomenon occurred in 15 to 20% of unconscious patients with brain damage.
Furthermore, the rate of diagnosis of cognitive-motor dissociation was higher in participants examined with fMRI and EEG, suggesting that multiple tests, using different approaches, may be necessary to correctly assess a patient’s level of consciousness.
“Some patients with severe brain injuries do not appear to understand the outside world. However, when assessed using advanced techniques such as task-based fMRI and EEG, we can detect brain activity that suggests otherwise.”explains the study’s lead author, Yelena Bodien, in a press release.
Cognitive-motor dissociation: a discovery that could change care
“These findings raise crucial ethical, clinical and scientific questions: How can we harness this invisible cognitive ability to establish a communication system and promote subsequent recovery?”the expert believes. She and her colleagues also note that knowing that a person is cognitively aware and has more abilities than they immediately seem can also change the clinical care they receive.
“Families have told us that once a positive test result revealing motor cognitive dissociation is shared with the patients’ clinical team, it can change the way the team interacts with their loved one.”explains Yelena Bodien. “Suddenly the team is paying more attention to subtle behavioral cues that might be under voluntary control, or talking to the patient, or playing music in the room.”
The specialist adds that “Failure to detect motor cognitive dissociation can have serious consequences, including premature withdrawal of life support and lack of access to intensive rehabilitation”.