On the occasion of the “Turquoise September” month of mobilization, specialists untangle the truth from the falsehoods about endometrial cancer.

- With more than 8,800 cases per year in France, endometrial cancer is the most common gynecological cancer after breast cancer.
- The main warning symptom is the presence of genital bleeding, even minimal, after menopause or outside of menstruation before menopause.
- Aging, overweight, obesity, diabetes, high blood pressure and never having been pregnant are the main risk factors for endometrial cancer.
A new communication campaign by the National College of French Gynecologists and Obstetricians, the Society of Gynecological and Pelvic Surgery, the French Society of Onco-Gynecology, the French Society of Oncological Surgery, the Women’s Health Fund and three patient associations is currently aimed at raising awareness of endometrial cancer. To do this, the experts analyzed a list of preconceived ideas circulating about this disease that is little known to the general public.
1) Endometrial cancer is rare.
Fake – With more than 8,800 cases per year in France, endometrial cancer is the most common gynecological cancer after breast cancer. 2,500 women die from it each year in our country.
2) There are no warning symptoms.
Fake – The main warning symptom is the presence of genital bleeding, even minimal, after menopause or outside of menstruation before menopause. This should lead to a rapid consultation with a gynecologist for examinations.
3) We know little about the risk factors.
Fake – Aging, overweight, obesity, diabetes, high blood pressure and never having been pregnant are the main risk factors. Of the 20 most common types of tumors, endometrial cancer has the strongest link with obesity.
4) It is a cancer of young women.
True and false – In 5 to 10% of cases, endometrial cancer affects women of childbearing age and, through the use of an expert center, it is possible to attempt to preserve fertility. However, the median age at diagnosis is 69 years with a peak incidence between 70 and 74 years.
5) Organized cervical cancer screening can detect endometrial cancer.
Fake – The endometrium is the lining of the uterus, not the cervix. In menstruating women, this lining thickens under the influence of hormones during the first part of the cycle. In the absence of fertilization, part of the endometrium is shed when menstruation occurs. If endometrial cancer is not detected and treated in time, it can spread to the uterine muscle or neighboring organs.
6) Endometrial cancer is difficult to treat.
Fake – This is a cancer with a good prognosis provided it is detected early, even if the effects of treatments should not be underestimated. A 90% cure rate is achieved at 5 years for cancers diagnosed at an early stage and 80% for stage 2 cancers.
7) Surgery is the preferred treatment for endometrial cancer.
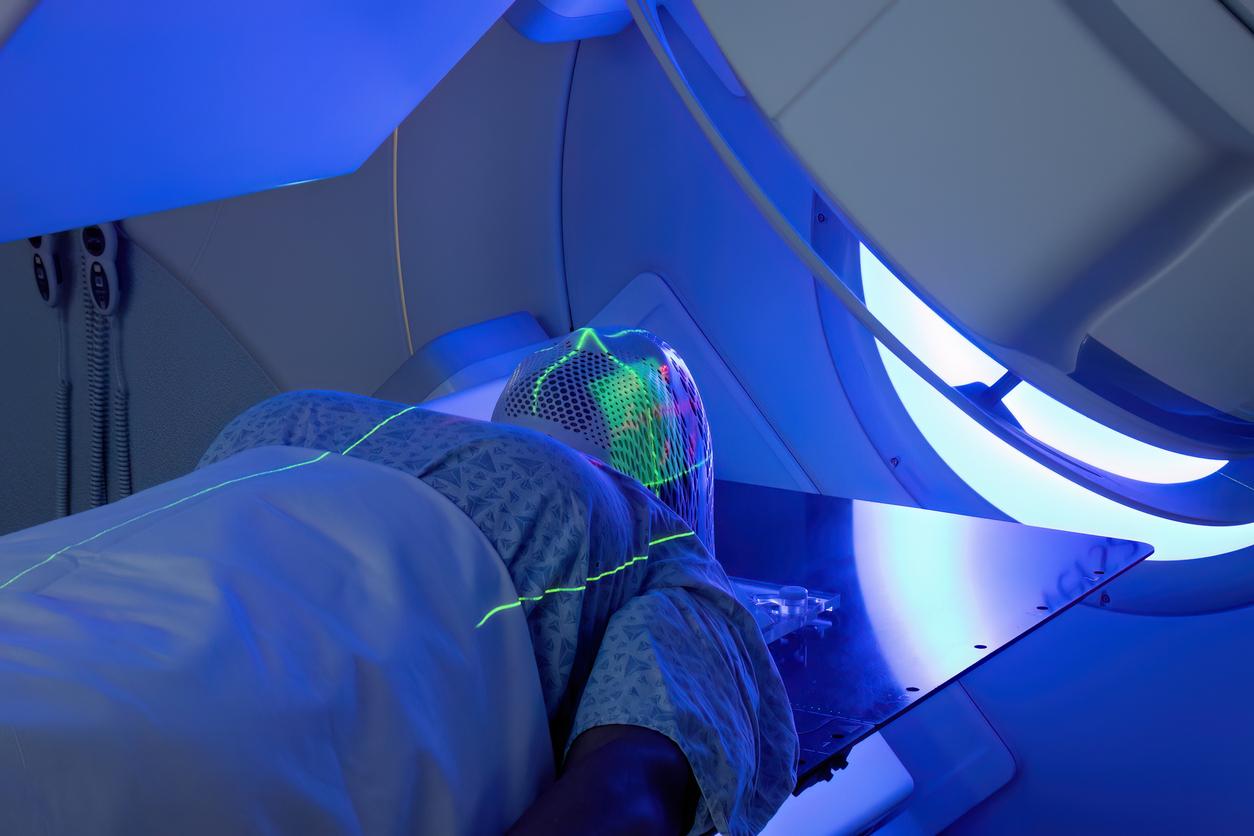
TRUE – Surgery is the first-line treatment for endometrial cancer and in 60 to 70% of cases, it cures patients. The procedure involves removing the uterus, ovaries and fallopian tubes. Minimally invasive techniques are preferred whenever possible (laparoscopic or robot-assisted).
8) Surgery is the only treatment for endometrial cancer.
Fake – Thanks to the molecular characterization of tumors, the proposed treatment will vary from surgery alone to a multidisciplinary approach including surgery, chemotherapy or immunotherapy.
9) Endometrial cancer research has stopped.
Fake – Promising studies on new avenues of research such as immunotherapy are multiplying with very encouraging results that could lead to a therapeutic de-escalation. Targeted therapies that attack specific metabolic pathways used by cancer cells to multiply in an anarchic manner are also showing very encouraging results.
10) Quality of life and intimate life are preserved after treatment.
True and false – Post-treatment after-effects too often continue to weigh on the daily lives of women who have suffered from endometrial cancer, particularly by impacting their intimate life. However, supportive care is now offered in most specialized establishments: nutrition-dietetics, adapted physical activity, oncopsychology, fertility/early menopause consultation, oncosexuality. A dialogue must be established with the care team and patient associations on these subjects as soon as possible.