In these times of intense heat, malignant exertional hyperthermia constitutes a vital risk in the event of prolonged and intense physical activity in hot weather.

- Malignant exertional hyperthermia is a life-threatening medical emergency.
- Treatment of malignant exertional hyperthermia is based on rapid management based on cooling the body.
- No physical activity in the heat and optimal hydration to avoid malignant hyperthermia during exercise.
It’s a potentially serious element that even the organizers of the 2024 Olympic and Paralympic Games have thought about: malignant exertional hyperthermia (or MHE).
Following intense physical exercise performed in adverse climatic conditions including heat and a certain degree of humidity (the more humid the heat, the less the body can eliminate sweat), exercise-induced malignant hyperthermia typically occurs in marathon runners. But although it generally occurs in amateur or professional sports, it is also common in workers, such as construction workers, in the middle of a scorching summer. It can also occur during leisure activities in full sun. And it is a true medical emergency that puts life at risk.
A rectal temperature that exceeds 40°C
Malignant exertional hyperthermia occurs during or immediately after intense and prolonged physical exercise. It can occur as soon as the heat exceeds 25 °C but also at lower temperatures in some people in poor physical condition or suffering from chronic diseases. The rectal temperature of the affected person is then higher than 40 °C and is accompanied by disturbances of consciousness.
During the day at the National Academy of Medicine on June 19, 2024 dedicated to the medicine of the Olympic and Paralympic Games, Dr. Stéphane Bermon, sports physician, exercise physiologist at the Monaco Institute of Sports Medicine and Surgery (IM2S), and medical director of the International Athletics Federation, specifies that “the‘impact [nombre de nouveaux cas d’une maladie apparus durant une période de temps donné, ndlr] is variable but can reach 10/1000 elite athletes in athletics “And outside of sports athletes, it is a little more important.
A vital prognosis engaged
Dr. Bermon recalls that during an HME ” the vital prognosis is engaged ” and that it exists ” 27% mortality if not properly managed “He mentions that we must be more and more careful.” given global warming “.
He specifies that “ L’exercise in a hot environment induces, as part of thermoregulation, a redistribution of blood flow to the benefit of skin tissues. There is therefore hypoperfusion of the digestive tract accompanied by a possible generalized inflammatory syndrome with coagulopathy [trouble de la coagulation, ndlr] “.
The manifestations of HME are often impressive with a ” very significant impact on the brain, as well as major polyvisceral failure [plusieurs organes se détériorent rapidement, ndlr] » which could lead to death.
Be alarmed at the first signs
The first signs of “heat stroke” should be a warning sign: feeling unwell, vomiting, intense thirst, cramps, headaches, dizziness, unusual behavior (aggressiveness, disorientation, etc.). You should act as soon as these first symptoms appear by calling emergency services, but also by cooling the person down: spraying them with water, putting them in the shade, ventilating them by providing a possible draft and reassuring them. If they vomit, they should be placed in the lateral safety position and reassured. However, they should not be given any medication. Emergency services will take care of this if necessary (including early intravenous hydration).
Act quickly
Without prompt and appropriate care, signs of encephalopathy, i.e. brain damage, appear quickly. They can range from confusion to coma, including convulsions..
Damage to muscle fibers (rhabdomyolysis) may also occur, causing pain (myalgia) and muscle weakness, as well as an abnormal presence of myoglobin (a protein found in muscle fibers) in the urine (myoglobinuria).
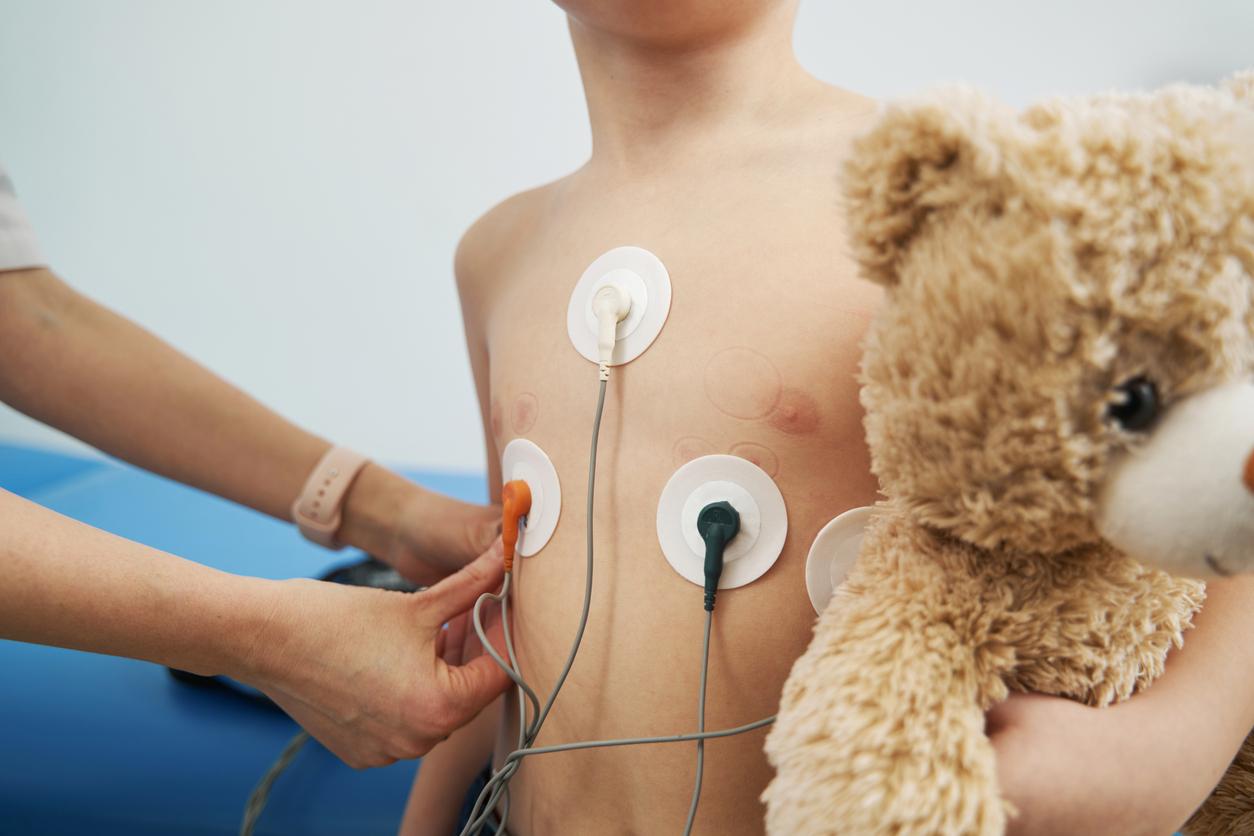
Other signs are present such as tachycardia or increased respiratory rate (tachypnea).
Dr. Bermon points out that “cerebral, cardiac and muscular complications are also possible in the long term.”

Cool immediately
Rapid treatment is essential. Immediate cooling of the affected person is a major element. This is done by immersion in cold water or, if this is not possible, by placing a refrigerated blanket or ice packs on the main vascular axes (axillary and femoral).
Dr. Bermon insists on the need for a ” cold bath (2 to 12 degrees) for 30 minutes, and the presence of at least 2 people because the person with HME generally has behavioral disorders which can make care difficult ” He specifies that it is necessary to ” monitor body temperature using a rectal probe “.
Risk factors to consider
According to Dr. Bermon, we must be vigilant about ” certain risk factors such as recurrent or recent infections, a history of HME (a person who has already had HME is more at risk of having it again), the elderly, a high BMI (body mass index) and/or fat mass, a lack of acclimatization to heat for which there are protocols of 8 to 10 days “.
The risk is also higher when the sport or physical activity is practiced during the hottest hours of summer, in the absence of wind or in the presence of hot wind, and in a humid environment. These climatic conditions do not promote the evacuation of heat through perspiration and are therefore a risk factor for HME.
Warning signs to watch out for
Let us remember that exertional malignant hyperthermia does not only occur in athletes. It can happen to any amateur athlete or even in the case of recreational physical activity (DIY, gardening, etc.) or professionally. The appearance of warning signs and discomfort should alert you and stop the activity in progress. Therefore, avoid physical activities in full heat and hydrate yourself well.