Autoimmune myasthenia has a considerable impact on the social and family life of patients. As the first European Day dedicated to it has just been held, insights into this disease with Dr. Saskia Bresch, neurologist.
– Why Doctor: The first European Day of Autoimmune Myasthenia has just been held. What is this disease?
Dr. Saskia Bresch: Generalized myasthenia gravis is an autoimmune disease, that is to say that the patient’s immune system produces antibodies which go to the level of the junction between the nerves and the muscles, preventing their proper communication and this leads to a muscle fatigue.
– What are the symptoms ?
There are several symptoms that can appear according to the different types of autoimmune myasthenia gravis. There are purely ocular forms that result in a drooping eyelid called ptosis and fluctuating double vision. And then there are generalized autoimmune myasthenia gravis which can affect other muscles. These are muscles that are called “voluntary”, that is to say that the patient controls himself. There there is fatigue in the arms, legs and there may also be respiratory impairment or swallowing impairment, which are two signs of seriousness. In this generalized myasthenia we find of course eye problems, also difficulties in chewing or articulating and changes in the voice.
– How many people in France does it concern?
The prevalence of these diseases is not well known in France, as for many rare diseases. But the ocular form is one of the most frequent forms compared to the generalized form.
– At what time of life can myasthenia appear?
You should know that myasthenia gravis can occur at any age, from birth to 90! But there are peaks in frequency around 30 or 40 years old and then around 60 years old. And this disease is often under-diagnosed because it is really on the statements of the patient that the diagnosis must be made. When you examine it, there is not much, especially when it is fatigue on exertion that you do not see in consultation.
But the two signs of seriousness that the patient must be aware of are difficulty breathing which can lead to severe respiratory failure and difficulty swallowing which can lead to choking. In the presence of these symptoms, he must go directly to the emergency room.
– What do we know about the causes of the disease?
The exact causes of this disease are not known. In fact, we don’t know where it comes from. Often patients have had an infection or vaccination that boosts the immune system, have had surgery, or have been under a lot of stress. But these are only triggering factors, the myasthenia was already there at the base. This disease can be there in an underlying way for years and after an event like the ones we have just mentioned, the symptoms appear.
– Is there a risk of diagnostic error for patients who have symptoms?
It is a disease on which there is still unfortunately a big diagnostic error. In the ocular form that manifests as ptosis, we see patients who undergo surgery one or more times thinking that it is an eyelid that falls with age and that having the operation will improve things. But in myasthenia, since it’s muscle fatigability, it will come back. When the patient has diplopia, that is to say double vision, then wandering is a little less frequent. For generalized forms, there are many patients who are not diagnosed because despite reports of fatigue, when the doctor examines there are practically no clinical signs. Either we think more of fibromyalgia, or we put their fatigue on the back of a form of laziness! I’ve seen patients 5-10 years after their symptoms started, and they’ve seen many doctors in between, including psychiatrists because they’ve been told it’s all in their head.
– How is the diagnosis made?
To make the diagnosis, it’s complicated anyway because all the para-clinical examinations can come back negative when the patient really has myasthenia. So we are often faced with a diagnosis based essentially on questioning.
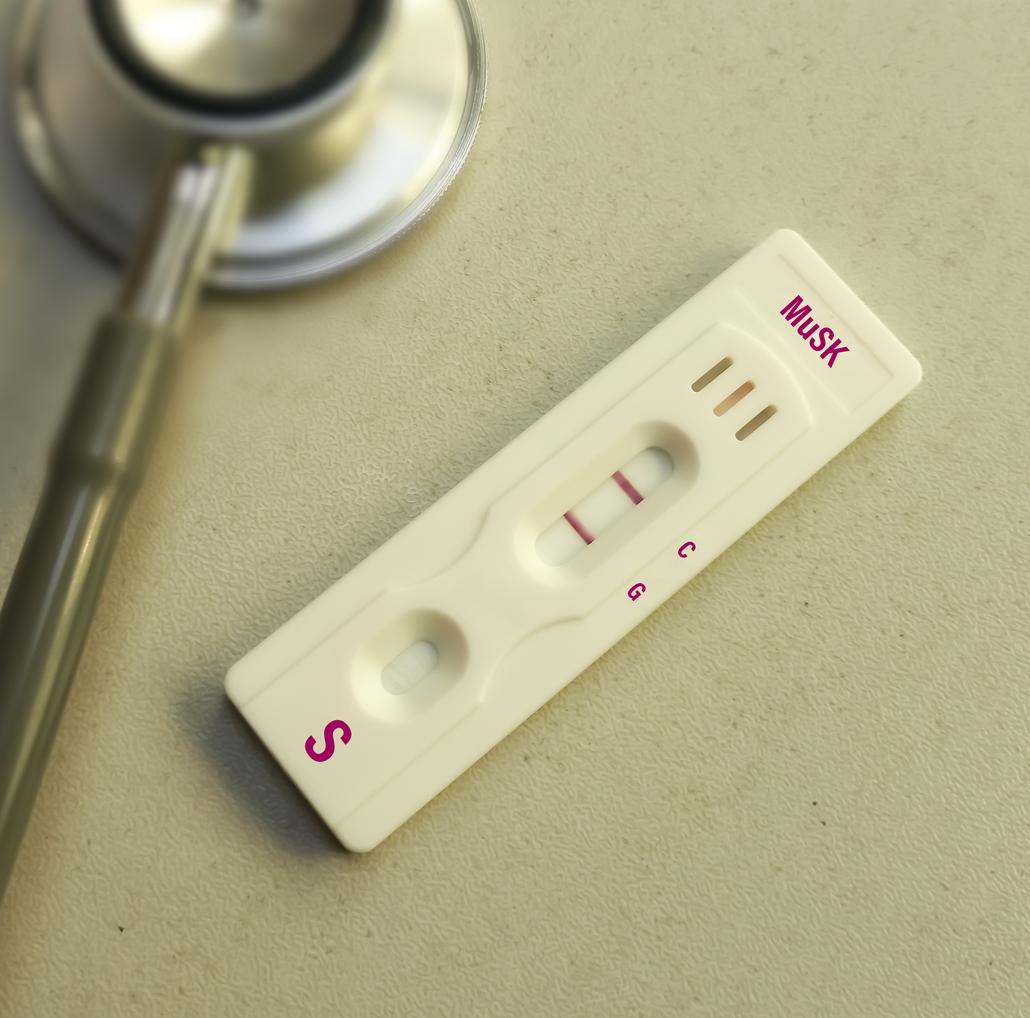
There are two major tests that are done for diagnosis. There are antibodies from a blood test but the level that identifies the disease is only present in a tiny percentage of cases. The second is the electro-myogram and it is also not very sensitive and when it is normal it does not eliminate the possibility of myasthenia.
– How do the different forms of the disease evolve?
For ocular myasthenia we only talk about it after the first two years because we know that within this period it can turn into generalized myasthenia. In the generalized forms, it is very variable. The disease can worsen in some patients in one or two months and they end up in intensive care – the disease can indeed be very severe and lead to death. And then for others, we see a somewhat chronic illness set in but without the risk of ending up in intensive care. But it is difficult to determine the prognostic factors. In any case, it is a disease that we have for life and even if we manage to improve the patients thanks to our treatments, it will always be necessary to monitor possible aggravations.
– What are the treatments for myasthenia gravis?
To improve the situation of patients, there are three categories of treatments. There are treatments for the symptoms including medications that are there to re-fuel the muscles. Then we have crisis treatments and especially when it is very severe and there is a vital risk, we use either immunoglobulins or plasma exchanges which are products that purify the blood of the antibodies responsible for the disease. It works well at the time but the aggravation can return after a month. And then we have the third category, long-term immunosuppressive treatments that attack the disease at its core by killing the white blood cells that make the antibodies. But they increase the risk of infection
– What impact can this disease have on other health problems?
The real issue is that there are many contraindicated medications that risk re-triggering a myasthenia crisis, such as anxiolytics, many antibiotics and beta-blockers. When a diagnosis of myasthenia is announced to the patient, he is given a card containing the list of contraindications that he must show as soon as he consults a doctor or pharmacist. It is very important that he understands that he himself is the safeguard because many general practitioners do not know myasthenia gravis and do not know how dangerous certain prescriptions can be.
– How is patient follow-up carried out?
It is a follow-up that is done by a neurologist and we have reference centers all over France with specialized neurologists. For a person who is doing well, this follow-up can be every three to six months, but at the start of the illness, it may be necessary to consult every week.
– Can autoimmune myasthenia gravis be considered a disabling disease?
This disease has a huge impact on the quality of life. These are symptoms that worsen with exertion, so the more patients want to do things, the more tired they will be. If they are not properly cared for, and sometimes even despite treatment, this fatigue means that many are forced to stop working, find it difficult to manage their daily lives. They are exhausted, they have a permanent screed and sometimes it is also very painful.

















