For the first time, researchers have identified a gene allowing the bacterium E. coli to escape antibiotics, which offers new prospects for treatment.

- The researchers discovered in the strain of E. coli ST131 the presence of a gene which makes the bacterium resistant to broad-spectrum antibiotics.
- This discovery will be able to lead to new treatments that are more suitable for countering the antibiotic resistance of the bacteria.
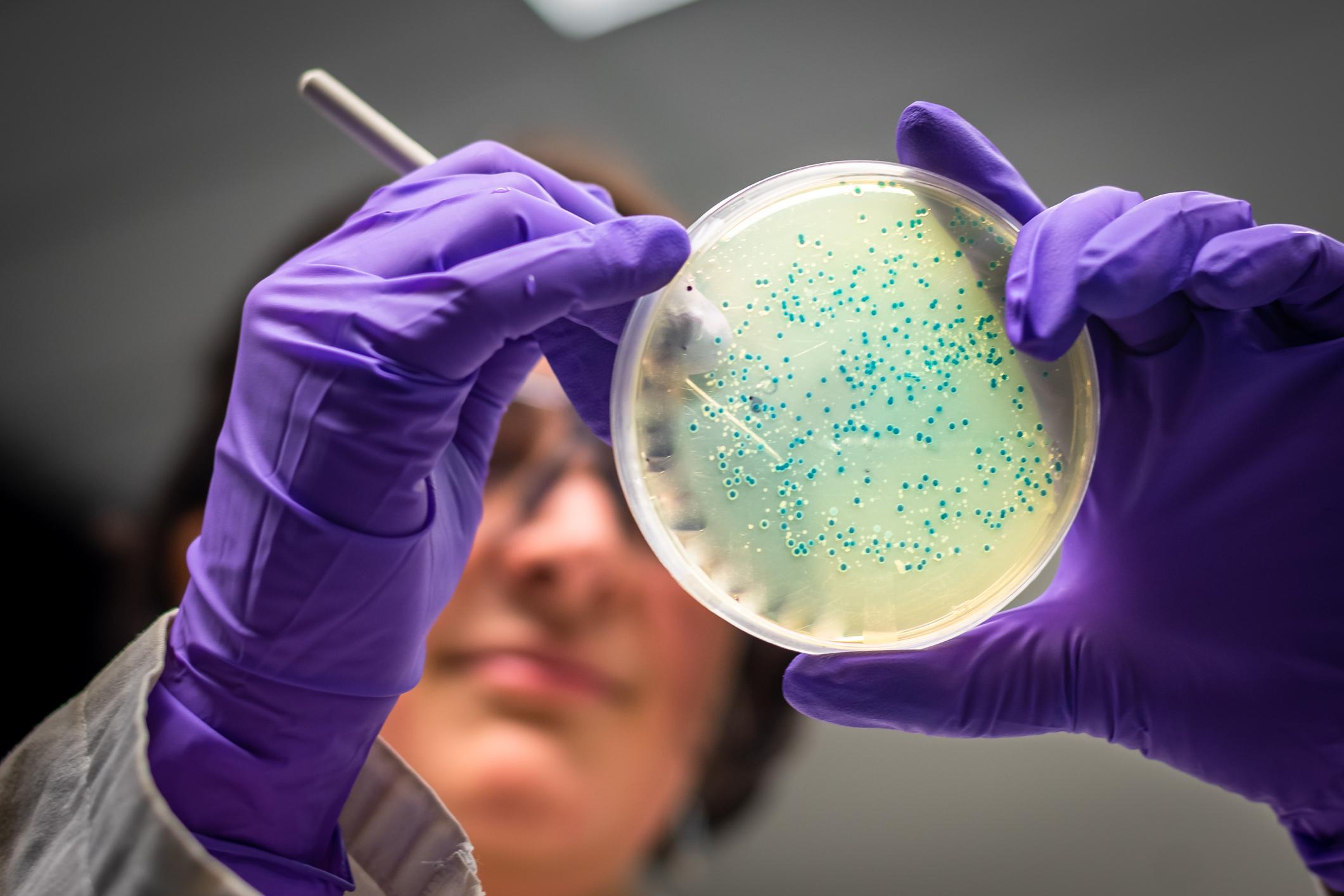
Naturally present in the intestine, the bacterium Escherichia coli (E. coli) is mostly harmless. But it happens that certain strains cause urinary tract infections, pneumonia and gastroenteritis. This is particularly the case of a multi-resistant strain called E. coli ST131, which can spread from the digestive tract to the female urinary tract through the urethra, and infect the bladder.
This multi-resistant strain is at the origin of a major discovery on this pathogenic agent. In a study published in the journal Antimicrobial Agents and Chemotherapyresearchers from the University of Queensland (Australia) discovered the presence in E. coli ST131 with a gene that makes it highly resistant to commonly prescribed antibiotics. According to Professor Mark Schembri, of the School of Chemistry and Molecular Biosciences at UQ, this “resistance gene” can also spread incredibly quickly. “Unlike gene transfer in humans, where sex is required to transfer genes, bacteria have genetic structures in their cells – called plasmids – that are quickly and easily exchanged between them.”
New strategies to fight infections
The antibiotics usually prescribed against an E. coli infection are broad-spectrum fluoroquinolones, used in particular against urinary tract infections, blood infections and pneumonia. However, the E. coli ST131 gene “works with other resistance genes to achieve higher level resistance to the highest antibiotic concentrations we can achieve during treatment”.
This discovery means, according to the researchers, that they will need “to create antibiotics capable of fighting against these infections despite this mechanism of antibiotic resistance”.
“We have lost a vital part of our arsenal to treat urinary tract infection and sepsis, but there is still hope, emphasizes Professor Schembri. Now that we understand the impact of this plasmid-mediated antibiotic resistance gene, we can develop more tailored treatment strategies. These could include new combinations of antibiotics, or even alternative non-antibiotic drugs that block E. coli ST131 infection.”
.