More and more bacteria are developing defense mechanisms that allow them to resist antibiotic treatments, transforming once benign infections into serious and potentially fatal diseases.

- Antibiotic resistance is a major public health problem that threatens the effectiveness of anti-infective treatments.
- Hospitals are particularly affected by this phenomenon due to the concentration of vulnerable patients and the intensive use of antibiotics.
- To combat antibiotic resistance, it is essential to implement rigorous prevention measures at the individual, institutional and societal levels.
Hospitals, due to the concentration of vulnerable patients and the intensive use of antibiotics, are particularly affected by this phenomenon.
Antibiotic resistance is a natural process of natural selection. Bacteria multiply at a very rapid rate, and as they multiply, genetic mutations can occur. Some of these mutations make the bacteria resistant to one or more antibiotics. When these resistant bacteria are exposed to an antibiotic, they survive and multiply, while the susceptible bacteria die. Over time, the bacterial population becomes increasingly resistant.
The 3 factors of antibiotic resistance
Several factors promote the emergence of resistance:
• Overuse of antibiotics : Excessive and inappropriate use of antibiotics creates selection pressure that favors the emergence of resistant bacteria.
• Nosocomial infections : Hospitals are environments conducive to the transmission of resistant bacteria, due to the concentration of vulnerable patients and the presence of numerous risk factors (contaminated medical equipment, healthcare personnel carrying resistant bacteria, etc.).
• The spread of resistance genes : Bacteria can exchange genes with each other, which facilitates the spread of resistance.
The consequences of antibiotic resistance are multiple and serious:
• Increased mortality : Resistant infections are more difficult to treat and increase the risk of complications and death.
• Extension of the duration of hospitalization : Patients infected with resistant bacteria require more intensive care and longer courses of treatment.
• Rising health costs : Treatment of resistant infections is more costly, due to the use of more powerful antibiotics and the need for strict prevention measures.
• Loss of therapeutic efficacy : If we fail to control antibiotic resistance, we risk returning to a pre-antibiotic era, when common infections could be fatal.
The challenges for hospitals
Hospitals are on the front lines of the threat of antibiotic resistance. They must implement rigorous measures to limit the spread of resistant bacteria:
• Strict hygiene : Washing hands, wearing gloves and gowns, and disinfecting medical equipment are essential actions to prevent infections.
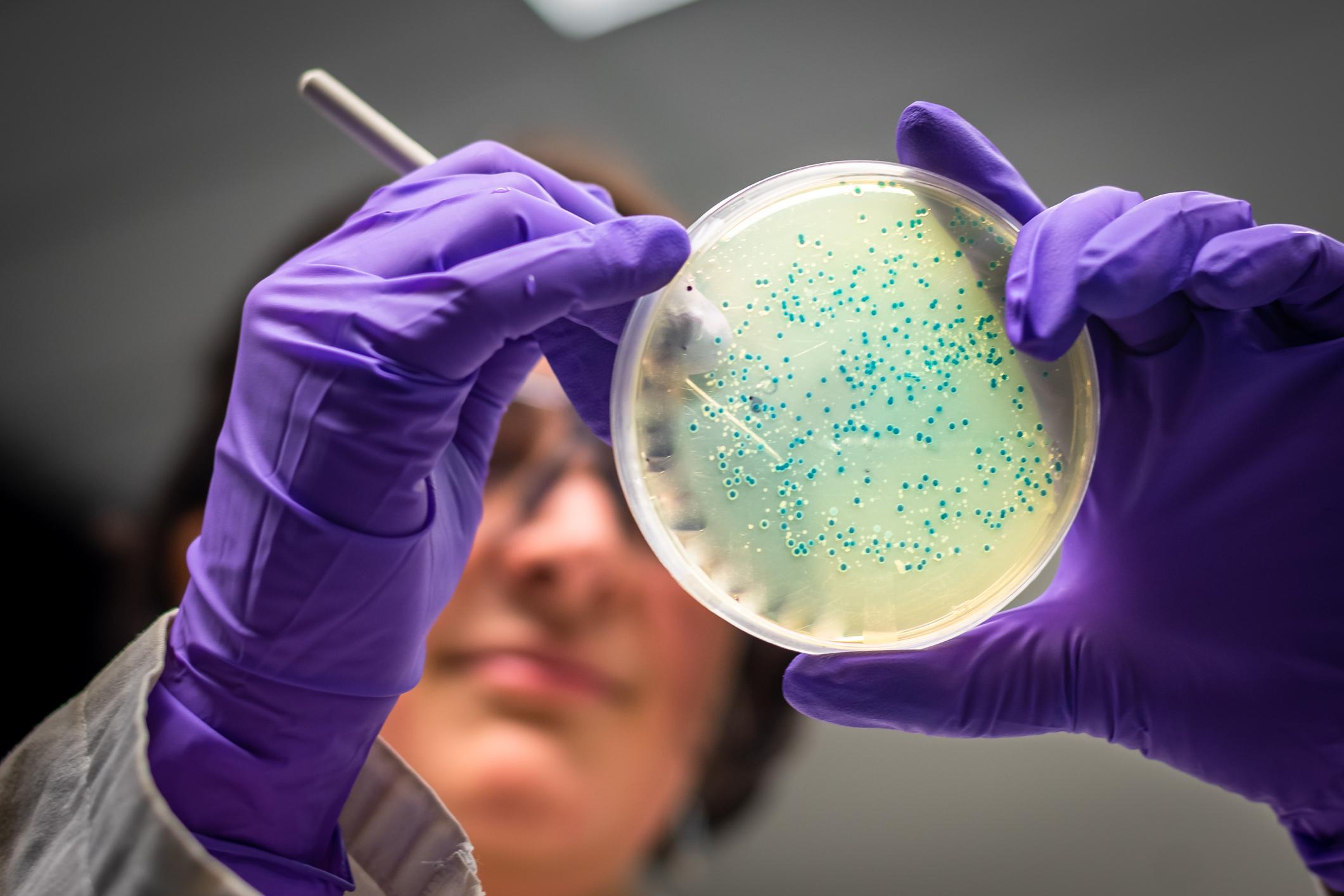
• Epidemiological surveillance : It is important to monitor the circulation of resistant bacteria in the hospital in order to quickly detect outbreaks of infection.
• A judicious prescription of antibiotics : Antibiotics should be prescribed in a reasoned manner, taking into account national and international recommendations.
• Implementation of programs to prevent healthcare-associated infections : These programs aim to reduce the risk of nosocomial infections and to limit the spread of resistant bacteria.
Antibiotic resistance is a major challenge for public health. To preserve the effectiveness of these essential medicines, it is necessary to raise awareness of this issue throughout society and to implement concrete actions to limit the spread of resistant bacteria.