During a study presented at the ASCO, which was held from May 29 to 31, French researchers show the interest of carrying out, in patients suffering from cancer of the cervix, first a biopsy of the sentinel lymph node before possibly carrying out a dissection if necessary.

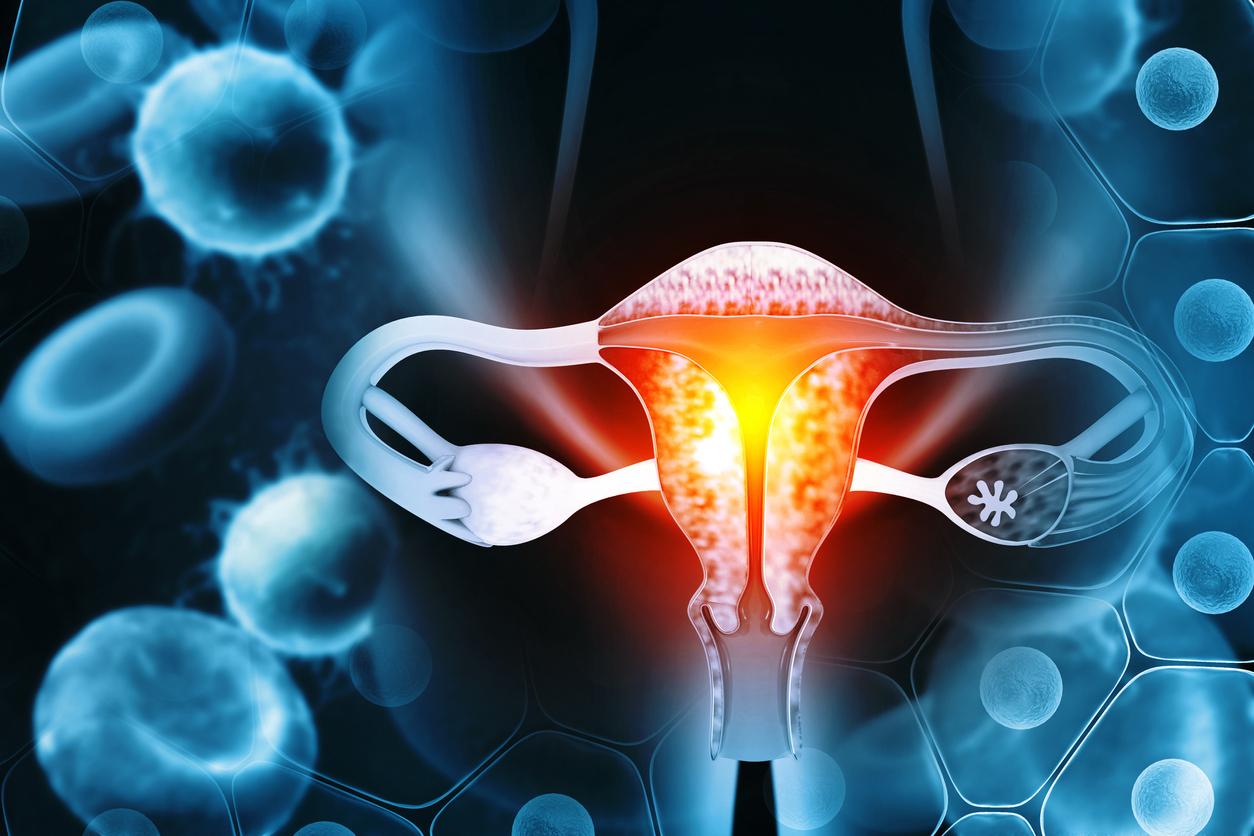
- During cervical cancer surgery, doctors usually perform a dissection of the lymph nodes in the pelvis.
- However, this procedure can sometimes lead to complications.
- Researchers at the Institut Curie therefore recommend a biopsy before any intervention of this type.
Cervical cancer is due in nearly 100% of cases to persistent infection with human papillomavirus (HPV), an infection transmitted through sexual contact. During their lifetime, eight out of ten women are exposed to the HPV virus. Worldwide, in 2018, about 570,000 the number of new cases of cervical cancer were diagnosed. In the same year, the disease is said to have led to 26,6000 deaths. In France, it is the twelfth most common female cancer and there are approximately 3,000 new cases each year. The 5-year survival rate is 63% and 59% at 10 years.
During surgery for cancer of the cervix, doctors generally carry out a dissection of the lymph nodes of the pelvis, that is to say the wide removal of all the nodes close to the tumor, in case the latter would be affected by tumor cells and could constitute a new cancerous focus.“But in 15% of cases, this intervention causes lymphedema of the legs: swelling, often painful and which can lead to other complications”, explains the Institut Curie. During I’American Society of Clinical Oncology, I’ASCOcongress which was held virtually from May 29 to 31, researchers presented the results of a study showing the interest of first performing a biopsy of the sentinel lymph node, closer to the tumor.
In recent years, this practice has become more and more common. It makes it possible to know in about 40 minutes whether the lymph node closest to the tumor is invaded or not by tumor cells. If so, a dissection is necessary because the tumor has already invaded the area. On the other hand, if the answer is negative, this invasive and risky intervention can be avoided. “The risk of occurrence [de complications, NDLR] depends both on individual factors such as obesity, pre-existing lymphatic circulation problems but also on the number of lymph nodes removed, the more radical the procedure, the higher the risk”, specifies Professor Lecuru, gynecological surgeon at the Institut Curie who presented the study.
“The new support standard”?
In the latter, he and his colleagues compared two international clinical trials (SENTICOL 1 and 2) conducted on approximately 300 women. Five years after treatment, the survival rate was the same in patients, whether they underwent a simple biopsy or bilateral dissection of the lymph nodes.
“However, we are still waiting four years from now for the results of the third component, SENTICOL 3, which is still in progress with 950 women in 12 countries.nuance Professor Lecuru. If the results are confirmed, the sentinel lymph node technique will become the new standard of care, which will considerably improve the quality of life of these patients”he hopes.
In France, women over the age of 25 are asked to take a smear every three years to detect cancer of the cervix as early as possible. From the age of 30, the High Authority for Health has recommended since July 2019 an HPV test every five years. For women not followed by a gynecologist, the High Authority for Health sends reminders to all those aged 25 to 65. But according to 20 minutes, too few patients would receive these letters. In addition, many regional bodies responsible for setting up screenings have not yet adapted to the new directives. As for the reimbursement of the HPV test for women aged 30 to 65, it has only been effective since April 2020.

.