Scientists have managed to quickly program natural viruses to kill two strains of E.Coli. This discovery represents a major advance in research against antibiotic resistance.
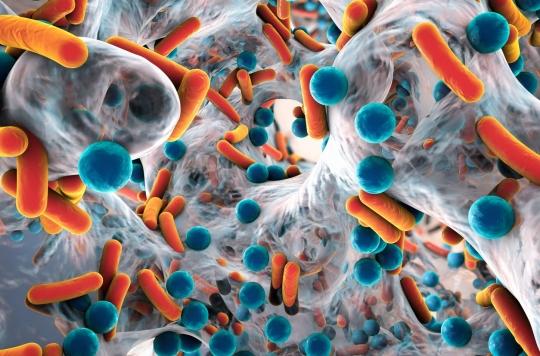
In recent years, antibiotic resistance has become a real public health issue. In 2014, in a surveillance report carried out on 114 countries, the WHO drew up an alarming observation: mild infections could kill again for lack of effective antibiotics. Many scientists have therefore been working on the subject for several years, trying in particular to deploy natural viruses called bacteriophages to infect and kill bacteria.
In the United States, the Food and Drug Administration has approved a few bacteriophages to kill harmful bacteria in food, but they have not been widely used to treat infections because finding naturally occurring bacteriophages that target the right type of bacteria can be a difficult and long process. In a study published on October 3 in the journal Cellresearchers announce however that they have succeeded in rapidly programming bacteriophages to kill two strains of E. coli thanks to mutations in a viral protein binding to host cells.
“As we increasingly see in the news, bacterial resistance continues to evolve and is becoming increasingly problematic for public health (…). (Bacterio)phages represent a very different way of killing bacteria than antibiotics, which is complementary to antibiotics, rather than trying to replace them,” said Timothy Lu, MIT associate professor of electrical and computer engineering and biological engineering, in the preamble to the study.
Viral “scaffolding”
To facilitate the development of these treatments, Lu’s lab therefore worked on viral “scaffolds” that could be easily reused to target different bacterial strains or different resistance mechanisms.
In 2015, researchers used a phage from the T7 family that naturally kills E.coli and showed they could program it to target other bacteria by swapping different tail fiber genes, which the bacteriophages use to latch onto. to receptors on the surface of host cells. They then wanted to find a way to speed up the process of adaptation of phages to a particular type of bacteria.
Modify the binding interaction with the bacterium
This time around, they managed to come up with a strategy that allowed them to rapidly create and test a much larger number of tail fiber variants. Already knowing that they are made up of segments called beta sheets connected by loops, they tried to mutate only the amino acids forming the loops, while preserving the structure of the beta sheet. “We have identified regions that we believe would have only a minimal effect on the structure of the protein, but which would be able to modify its binding interaction with the bacterium”, explains Professuer Kevin Yehl, the one of the authors of the study.
The researchers therefore created phages with around 10,000,000 different tail fibers and tested them against several strains of E. coli that had evolved to resist the unmodified bacteriophage. And while E.coli can become resistant to bacteriophages by mutating LPS receptors, researchers realized that their modified phages were able to kill even strains of E.coli whose LPS receptors were mutated.
“It’s only a beginning”
Building on these results, the researchers now plan to apply this approach to target other resistance mechanisms used by E. coli. They also hope to develop phages capable of killing other types of harmful bacteria. “This is just the beginning, as there are many other viral scaffolds and bacteria to target,” explain the researchers who also plan to use bacteriophages to target specific strains of bacteria found in the human gut. cause of many health problems.
This summer, researchers at the University of North Carolina in the United States had already shown that modifying an already existing drug could make it possible to develop a stronger product, capable of attacking staphylococci aureus which can survive in environments with little oxygen, resistant to methicillin (MRSA), tobramycin or persistent staphylococci.
At the end of September, scientists from the University of Surrey (United Kingdom) then showed that combining epigallocatechin, an antioxidant present in green tea, with aztreonam, regularly used to treat infections caused by the pathogenic bacteria Pseudomonas aeruginosa, would help overcome the latter, which is now resistant to many classes of antibiotics.
.