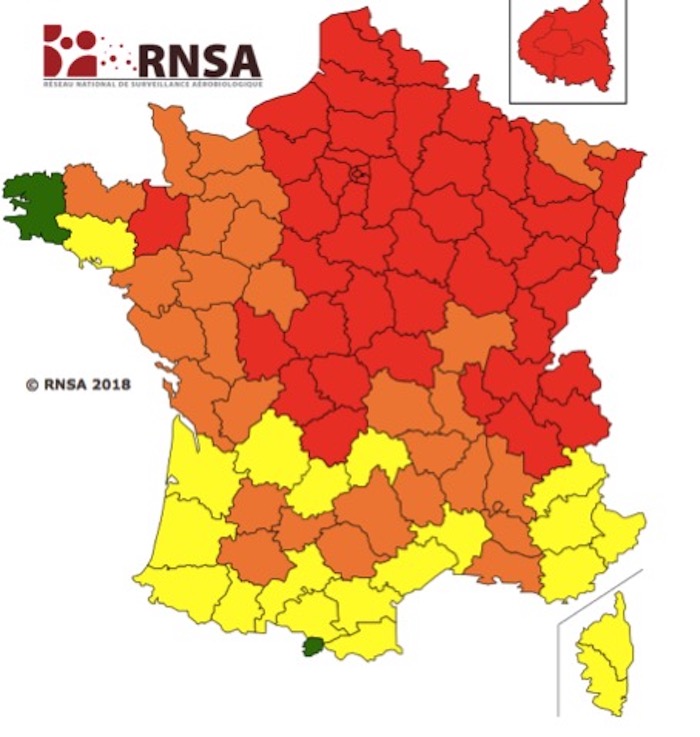
It’s suddenly spring, the return of heat, flowers, and pollen! In recent days the quantities have exploded in France. In the North, birch pollen is very present, in the South it is plane tree pollen. Dirty. time for allergy sufferers, unless they’ve prepared.

A favorable anticyclone, the arrival of spring, the conditions are met for the pollen grows. Everywhere in France, the quantities of pollen in the air are increasing. In the North, it is birch pollen that is very present, in the South plane tree pollen. For these two, the allergic risk is very high.
Throughout France, the risk of allergy is high for ash pollen. Hornbeam pollens could also reach this level in a few days. In the Southwest, the risk is medium for grass pollen, even if they are always present.
What is birch pollen allergy?
Birch pollen allergy is common and it is not necessary to have one in your garden: the birch trees of the surrounding 30 kilometers disperse this pollen which causes allergy symptoms. As with the allergy to pollen from other trees, this seasonal allergy manifests itself in the spring, now in April.
Other trees like beech, oak, maple and poplar also cause seasonal respiratory allergies in the spring. The components of alder pollen are very similar to those of birch, and if you are allergic to birch, you are usually allergic to alder pollen as well.
How does allergic rhinitis manifest?
Most often, the person who suffers from allergic rhinitis complains of nasal congestion which can lead to an obstruction of the nose (“stuffy nose”) and to irritation of the nose: “runny nose” (or “rhinorrhea”), sneezing, “itchy nose” or “itchy nose” (“nasal pruritus”).
Nasal congestion can be accompanied by sneezing, coughing and eye irritation (“allergic conjunctivitis”) with red, watery eyes.
It is not uncommon for tingling of the tongue and lips when eating apples, pears or celery, for example, to be the first indication of an allergy to birch pollen. Hazelnuts and peanuts can also be implicated in this type of allergic reaction linked to birch allergy. This is oral allergy syndrome or pollen-food syndrome related to birch allergy.
The impact of allergic rhinitis can cause sleep disorders with fatigue and irritation. People with allergic rhinitis often have a family history of allergy.
Should we suffer in silence?
Like other respiratory allergies, the existence of allergy to birch pollen or that of other trees, especially if only the symptoms are treated, increases the risk of the development of other respiratory allergies and especially sensitization of the lungs. with allergic asthma, which is found in 20-25% of cases. Allergic asthma causes coughing, wheezing, shortness of breath and tightness.
Allergy testing is needed to confirm a diagnosis of respiratory allergy such as birch or other tree allergy, and initiate appropriate treatment.
These allergy tests are generally carried out on the skin (skin tests or Prick-tests) but can also be carried out in the form of serological tests (blood = dosage of specific IgE).
In certain situations, particularly those where skin tests show several positivities, molecular allergy tests may be used to confirm an allergy to birch pollen (family of plant stress proteins called PR-10).
How to protect yourself?
If you are allergic, a few precautions can help you. It is better to avoid walks in the forest, field or meadow when the allergic risk is high. If you are driving, you must close the windows. For the ventilation of the house or apartment, prefer the morning before sunrise and the evening after sunset to open the windows, pollens are more present in the middle of the day. Above all, it’s time to follow your antihistamine treatment!
What is the treatment for allergic rhinitis?
Systematic avoidance of the allergen is not always possible, but the treatments available are effective and generally safe, if used correctly.
It is recommended to take them systematically, every day, from the start of the signs and for the entire duration of the flowering in question. In some cases, it is possible to take them even a little before, which avoids letting it go and “chasing after the allergic inflammation” and blocking it from the start.
Oral antihistamines are the first-line drugs for allergic rhinitis. The oldest antihistamines have a potentially dangerous sedative effect when driving a car or in certain occupations. Second-generation antihistamines do not have a sedative effect and are now recommended as first-line treatment for people who must take this type of medication: desloratadine, fexofenadine, loratadine, cetirizine… Do not hesitate to try several of them in order to to find the molecule that best suits each person: there is indeed a strong individual susceptibility.
Nasal topical corticosteroids are the recommended first-line treatment for moderate or severe rhinitis (budesonide, fluticasone, mometasone, etc.). They are recommended as second-line treatment in patients with mild allergic rhinitis. Their regular use can even repair the effects of inflammation. Nasal corticosteroids have few side effects, but they can cause nose irritation or bleeding in 10-20% of people.
Nasal topical corticosteroids are superior to oral antihistamines for the treatment of allergic rhinitis. They offer a particularly significant advantage over antihistamines in people with perennial allergic rhinitis who suffer from moderate or severe nasal congestion. In this case, they must constitute the main treatment.
It is possible to combine topical corticosteroids with antihistamines.
In eye drops, topical corticosteroids are effective in the treatment of eye allergy (“conjunctivitis”).
Antileukotrienes can be used in the prevention of rhinitis, mainly in asthmatic people with naso-sinus polyposis.
Oral corticosteroids are not recommended because of the side effects that occur at doses where they are effective.
Avoid decongestant nasal sprays containing phenylephrine, which pose a risk of stroke.
Can birch allergy be cured?
To change the course of the allergic disease, it is possible to use specific immunotherapy, or “desensitization”: this technique makes it possible to induce tolerance to one or more allergens. The progress of recent years has reinforced the effectiveness of these treatments with better purification of allergens and the administration of some by the sublingual route. Subcutaneous injections take place once a week for 3 months, then once a month for 3 years.
Subcutaneous immunotherapy helps control the signs of allergies in more than two-thirds of people with allergic rhinitis and prevents the development of bronchial asthma and broadens the spectrum of allergies to other allergen over time. Desensitization works all the better when it is initiated soon after the development of the signs. In case of recurrence after desensitization, if the first immunotherapy was effective, it is possible to repeat it.
An interesting alternative is sublingual immunotherapy which must be started at least a few months before the pollen season: it is interesting not only for the treatment of the symptoms of birch allergy but also for changing the course of the allergic disease.
.


















