Many preconceived ideas, often unfounded, sometimes proven, revolve around endometriosis, a disease which affects at least one in ten women of childbearing age. Yasmine Candau, president of the EndoFrance association, disentangles the truth from the falsehood.

Having suffered from endometriosis for many years herself, Yasmine Candau is president ofEndoFrance for twelve years. The association, created in 2001,’s mission is to support people with endometriosis and those around them, to inform the general public about the disease, as well as to work with health professionals and public authorities to improve the Care course.
Why Doctor: What is endometriosis?
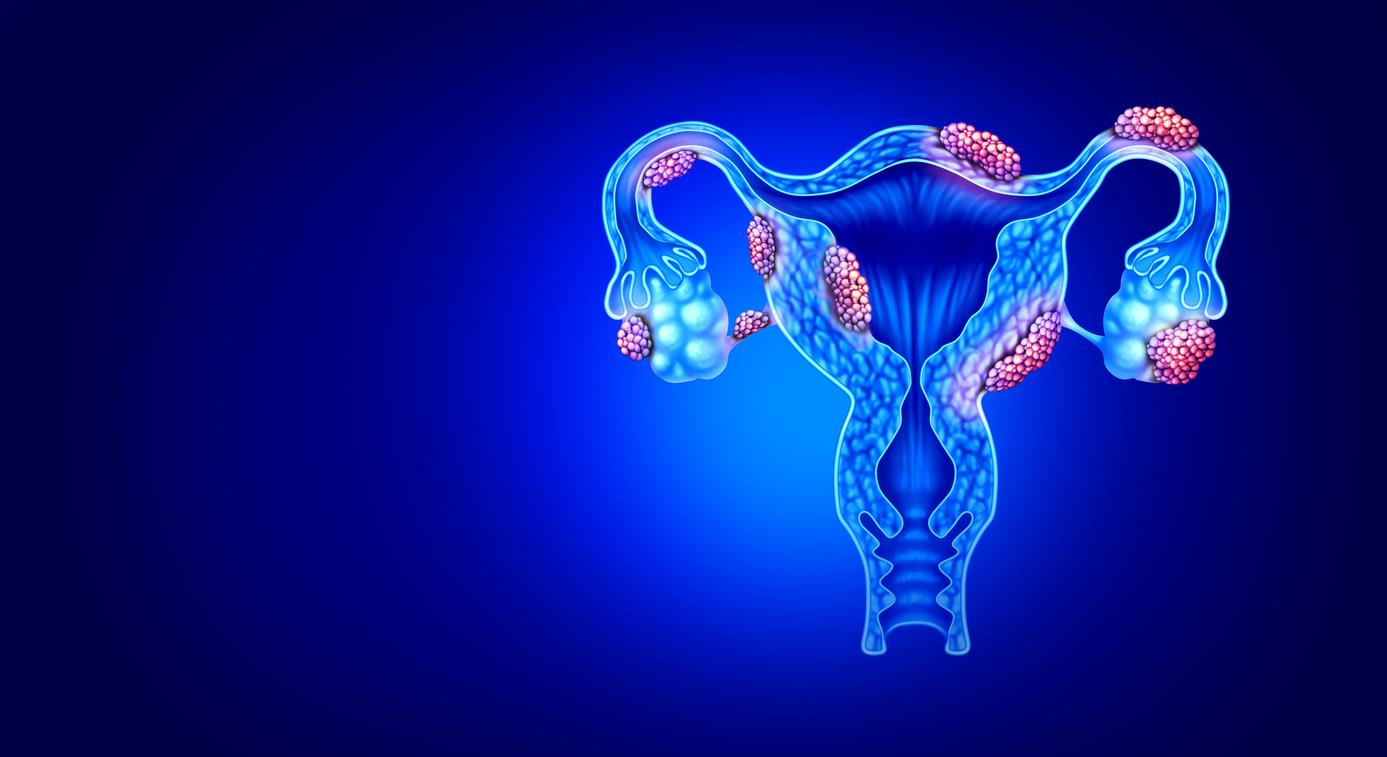
Yasmine Candau : It is a disease which takes its name from the endometrium, the mucous membrane which lines the uterus and which, at the time of the menstrual cycle, will swell in order to accommodate an embryo. When fertilization does not occur, this mucous membrane will slough off and bleed, which will cause periods. We speak of endometriosis when we find, elsewhere than in the uterine cavity, cells similar to this endometrium which are grafted onto organs such as the peritoneum, the uterus, the ovaries, the tubes, or even the bladder, the intestines. , the colon, the rectum and sometimes even the diaphragm. This will create cysts, nodules, adhesions. Every month, cycle after cycle, these lesions will also start to bleed. However, these microhemorrhages, which have no way to escape, will remain in the abdomen and trap the organs, which will cause severe pain linked to the inflammation.
It is a complex disease which has different symptoms: there are as many cases of endometriosis as there are people affected. Some have superficial forms (which will remain on the surface of the peritoneum, the membrane which surrounds our organs in the stomach), others deeper (the organs will be infiltrated by the lesions). Still others create cysts on the ovaries. There is also a very specific form called adenomyosis, when endometriosis develops within the uterine muscle itself.
Misconception #1: “It’s normal for periods to be painful”
Period pain is not normal if it is not relieved by basic analgesics, if it returns stronger and stronger each month and if it prevents you from acting on a daily basis. It’s not normal for a young girl to be unable to go to high school because of painful periods. This trivialization of pain has led to medical wandering which has meant that, until then, it took around seven years to diagnose the disease. What is normal, however, is that to evacuate the endometrium and menstrual blood, the uterus contracts, which can hurt, but this pain is relieved by medication. It is only if it persists that you should consult.
There are as many cases of endometriosis as there are people affected.
Misconception #2: “Endometriosis is a psychosomatic illness”
This has long been the opinion of the medical world. Although it can have disabling consequences, endometriosis is by definition a benign disease, which is not life-threatening. As a result, doctors, particularly general practitioners, are not trained and do not know how to refer patients complaining of chronic period pain. And given that medical imaging often reveals nothing abnormal, many consider that the illness is psychosomatic, “in the head”. We had to wait until 2020 for the decree to integrate endometriosis into second-cycle medical studies to appear, so it will still be a few years before doctors are truly trained in it. The strategy to combat endometriosis launched in 2022 should also help to fill this medical gap.
Misconception #3: “Endometriosis makes you infertile”
Endometriosis does not rhyme with infertility, but it is a risk factor and can sometimes lead to infertility: it is estimated that 40% of cases are due to endometriosis. Indeed, when we have several organs which are stuck together by adhesions and cysts altering their proper functioning, there are obviously mechanical difficulties in procreating. The reason is also chemical: the inflammation in the belly will release a lot of harmful enzymes, harmful to reproduction. Finally, endometriosis, depending on the location of the lesions, can cause intense pain during sexual intercourse. However, if we are afraid of having pain, we have less intercourse and therefore less chance of procreation…
Pregnancy does not cure endometriosis, it only puts it to rest.
Misconception #4: “Pregnancy cures endometriosis”
No, it’s simply that it allows the patient with endometriosis to “breathe” a little… Pregnancy is a natural amenorrhea (absence of periods) which will normally last nine months, during which the lesions will stabilize, or even decrease, at least “shut up”. Pregnancy does not cure endometriosis, it only puts it to sleep – and the disease awakens with the return of childbirth.

Misconception #5: “There is no treatment for endometriosis”
There is no cure for endometriosis, and most of the time the disease progresses. In a third of cases, however, it can be stabilized or even reduced thanks to drug treatments (analgesics or hormones) or surgical interventions intended to free the organs. Alongside this medical care, all supportive care can improve comfort and quality of life: osteopathy, acupuncture, physiotherapy, hypnosis, etc. Certain adapted sports are even recommended, such as walking, yoga or swimming. , in order to put his body and therefore his organs in motion.
All supportive care can improve comfort and quality of life: osteopathy, acupuncture, physiotherapy, hypnosis, etc.
Misconception #6: “If you don’t see anything, it’s because there’s nothing”
If it is barely developed, endometriosis may not be seen on imaging. But a normal ultrasound or MRI does not mean there is no endometriosis. Sometimes this only measures a few millimeters and radiologists, who are not sufficiently informed, can miss it. Hence the interest in meeting a doctor who will nevertheless offer a therapeutic trial to patients.
Misconception #7: “Endometriosis only affects adults”
No, it’s a disease that begins with menstruation, at puberty, and theoretically ends with menstruation, at menopause. Today there are more and more young girls diagnosed at the age of 18 or 19, whereas it was later a few years ago.
The pain of endometriosis begins during menstruation, but over time, the pain ends up becoming chronic if it is not stopped.
Misconception #8: “Endometriosis only causes pain during periods”
The pain of endometriosis begins during menstruation. But over time the pain ends up becoming chronic if we don’t stop it: the neurotransmitters will always send a painful signal to the brain, and if we don’t do anything to stop this message, it will continue to send it and the pain will become chronic. Some women can thus have pain at any time of the cycle: in particular during their periods, but also before and after. Some complain of having pain 25 days a month… This is where specific medications prescribed by algologists (pain doctors) or non-drug techniques (hypnosis, sophrology, neurostimulation) must be used. electric…) to relieve pain.