No, tuberculosis has not disappeared: according to the World Health Organization (WHO), this infectious pathology caused the death of 1.5 million people worldwide in 2014, and a third of the world’s population is thought to be a carrier of Koch’s bacillus, the bacterium that causes the disease.
In France, in 2014, 4827 new cases of tuberculosis were diagnosed (7.6 cases per 100,000 inhabitants); 36% of cases were in Île-de-France.
If tuberculosis indeed seems to be on the decline, “it’s a hydra waiting for us to let our guard down to come back in force” says Dr. Philippe Laurent, pulmonologist. “Tuberculosis is only kept under control thanks to very strict screening measures and Anti-Tuberculosis Centers (CLAT) distributed throughout the country: it’s a fight.“
What is tuberculosis?
Definition. Tuberculosis is an infectious disease caused by bacteria, Mycobacterium tuberculosiswhich is also called “Koch’s bacillus” in honor of Dr. Robert Koch, the German doctor who identified the pathogen in 1882.
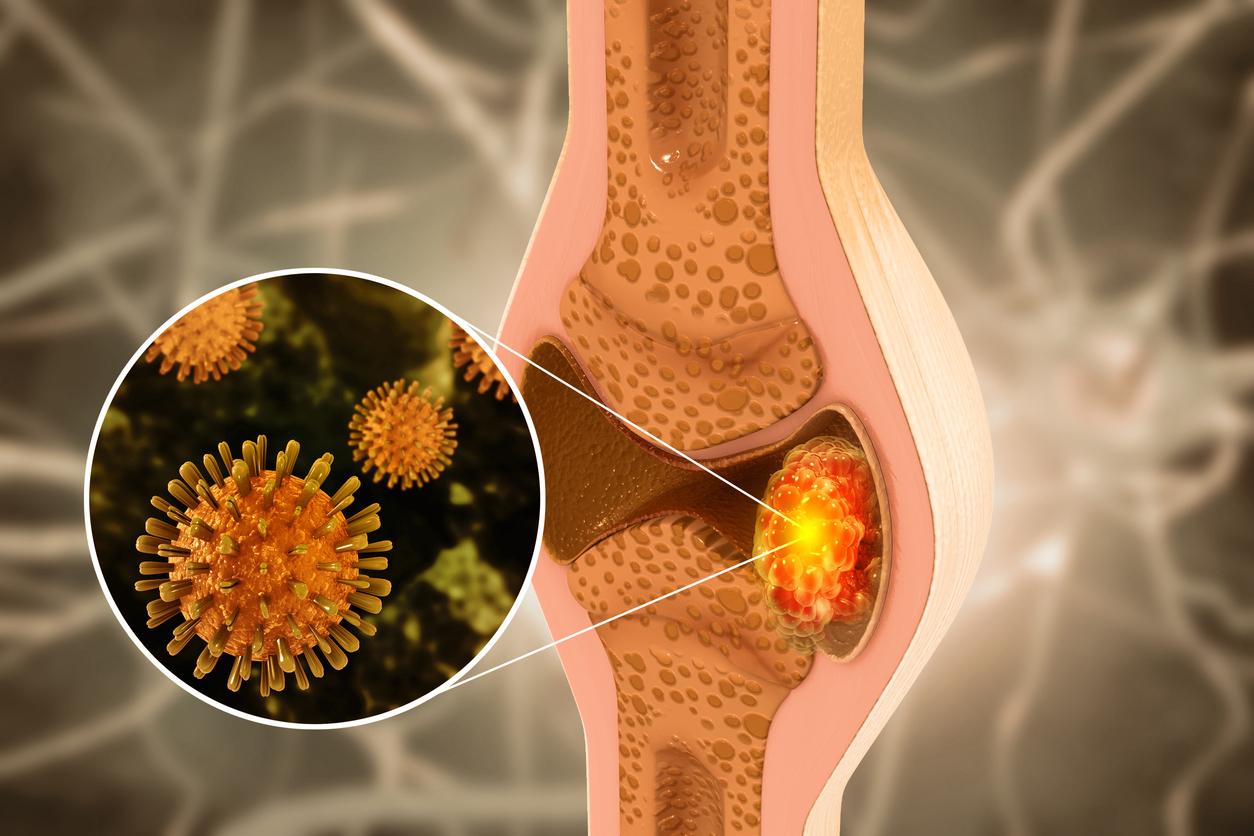
Transmission. Koch’s bacillus enters the body through the respiratory route: like the SARS-CoV-2 coronavirus, transmission takes place through sputters, sputum and droplets that are projected when speaking, coughing and when sneezing. Inserm estimates that 1 infected and untreated patient can contaminate 10 to 15 other people in the space of a year.
Once in the body, the bacterium lodges in the lungs and there are then 3 possibilities:
- Either the immune system manages to eliminate it completely,
- Either the disease starts: “if tuberculosis can start in anyone, the immunocompromised people who suffer from AIDS (untreated) or who are under immunosuppressive treatment (immunotherapy, biotherapies, etc.) are particularly concerned“says Dr. Laurent,
- Either the bacterium remains “dormant” in the body: “the disease can then be triggered 10, 20 to 40 years later, taking advantage of a period of immunosuppression or aging“adds the specialist. This is the most frequent case.
Tuberculosis: who is affected?
Everyone is susceptible to infection with Koch’s bacillus. However, some populations are at greater risk: “there are endemic regions where the bacterium circulates more: in France, this is the case of Île-de-France, Mayotte and Guyana“ remarks Dr. Laurent. The most precarious (homeless, for example) also have an increased risk of catching the bacteria. Mycobacterium tuberculosis.
In 2014, according to Inserm, the highest number of new cases was recorded in Southeast Asia and the Western Pacific region (58% of new cases). Africa however has the highest incidence with over 281 cases per 100,000 population in 2014.”Immigrant populations and travelers from these regions are more at risk of carrying Koch’s bacillus“ underlines the pulmonologist.
Tuberculosis: what are the symptoms?
In 90% of cases, after infection with Koch’s bacillus, the pathogen remains “dormant” in the body: there are therefore no symptoms. When the disease starts, we observe the appearance of non-specific symptoms:
- A fatty or dry cough: chronic, this can be accompanied by bloody sputum (sputum),
- significant fatigue,
- An alteration of the general state: feeling of weakness, weight loss…,
- pain in the chest,
- Low but persistent fever.
To know. In about 15% of cases, the disease (initially localized in the lungs) can spread to other organs: “we can then observe very severe forms, such as the dreaded tuberculous meningitis (which corresponds to neurological damage) but also lesions in the liver or bones (Pott’s disease, for example, damage to the thoraco-lumbar spine)“adds Dr. Laurent.
Tuberculosis: is it serious, doctor? Yes. “Tuberculosis is a disease that gradually “nibbles” the lungs: left untreated, it leads (more or less quickly) to respiratory failure. Not to mention the more severe (and also rarer) forms that spread to other organs, usually very severe” replies the doctor.
Diagnosis: how is tuberculosis detected?
Tuberculosis screening is offered in two situations: when a case of tuberculosis is detected (whether the disease is declared or not), screening is offered to the patient’s contact cases to limit the transmission of the bacterium. In addition, tuberculosis screening is aimed at targeted populations (migrants from endemic areas). It is carried out in the Tuberculosis Centers (CLAT).
“Tuberculosis screening consists of an IDR test (tuberculin skin test) or its blood equivalent and is intended for people who have not been vaccinated. Concretely, the IDR test corresponds to a small subcutaneous injectionexplains Dr. Laurent. If the patient has previously been infected with Koch’s bacillus, a skin reaction appears.“
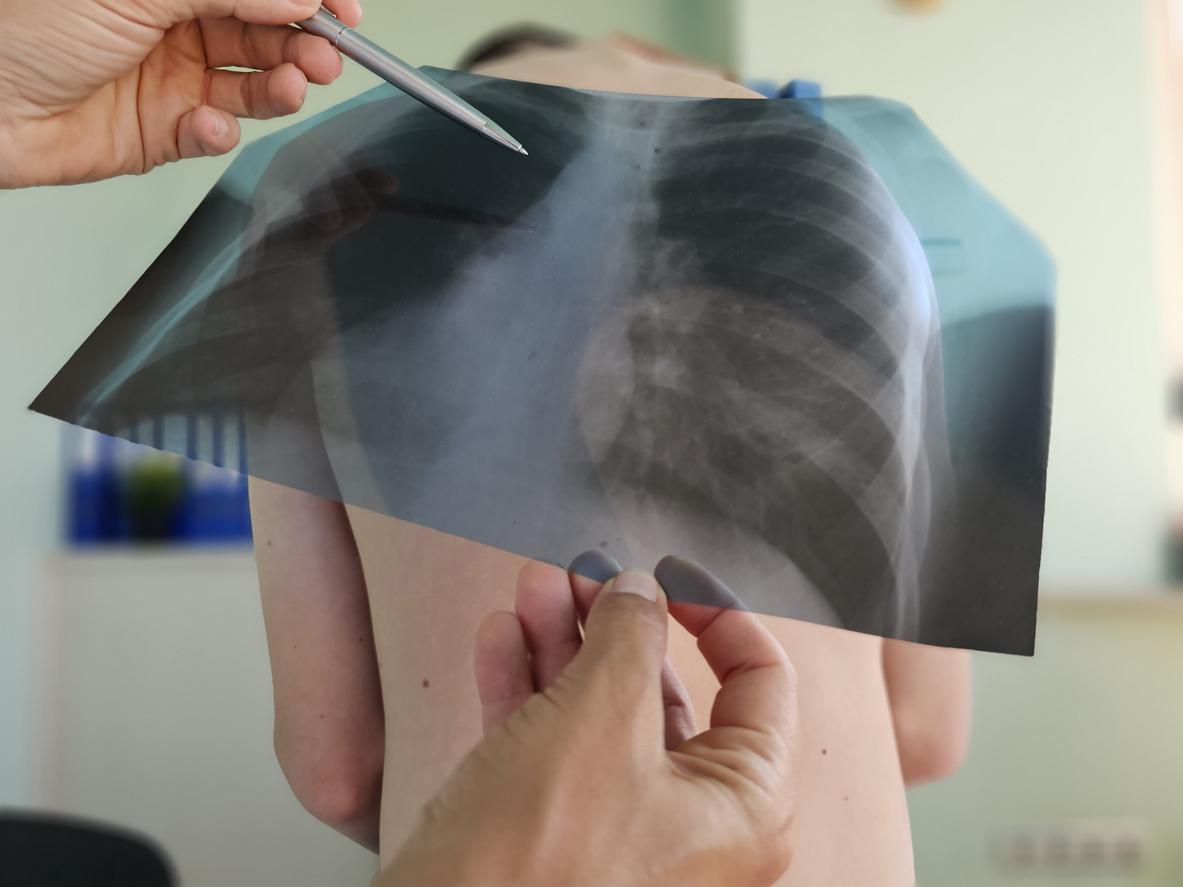
In case of symptoms, the diagnosis of tuberculosis first passes through a medical imaging examination: “an x-ray of the lungs and/or a CT scan of the thorax is carried out to observe possible lung damage“. To confirm the diagnosis, it is a question of identifying the germ in the sputum (understand: in a sputum) or in a lung sample (possibly carried out by fibroscopy).
Treatments and prevention: how is tuberculosis treated?
To know. Tuberculosis has been a notifiable disease since 1964.
- If the disease is declared (symptomatic)
First reflex: isolate the patient suffering from tuberculosis to limit the transmission of Koch’s bacillus to those around him. “If it is a severe form, isolation is done in the hospital for 15 days to 3 weeks” notes Dr. Laurent.
Antibiotic therapy which combines 3 antibiotic drugs (among them rifampicin, isoniazid, pyrazinamide and ethambutol) is then implemented for approximately 6 months. “The treatment is long because the germ is “hidden” in the cells“says the pulmonologist.
Effective, this antibiotic treatment can however cause undesirable effects: liver toxicity (hepatotoxicity), increase in uric acid levels (hyperuricemia), reduction of the visual field (toxicity for the optic nerve)…
- If the disease is latent (“dormant”)
The proposed anti-tuberculosis treatment is based on monotherapy or dual therapy, that is to say one or two antibiotics in combination. The duration of treatment is shorter, between 3 and 6 months. To note : “when the bacterium is “dormant” in the body, an onset of the disease is most often observed within two years“explains the pulmonologist.
To know.Koch’s bacillus is a bacterium that is beginning to become antibiotic resistant. In some cases, specific antibiotic therapy (with drugs that “bypass” antibiotic resistance) is necessary.
Prevention. In addition to targeted surveillance and screening around cases, the prevention of tuberculosis involves vaccination. Developed in France, the BCG vaccine has not been compulsory for young children since 2007, except in Guyana and Mayotte: with an effectiveness of between 75% and 85%, it “especially protects against severe forms of the disease“says Dr. Laurent. Vaccination is done in a single dose: it can be offered until the age of 15 for children at risk – who live in an endemic area, in particular.
“Wearing a mask and barrier gestures (social distancing, etc.) are also very effective in protecting against Koch’s bacillus.“
Thanks to Dr. Philippe Laurent, pulmonologist at the Aressy medical and cardiological clinic in Pau (ELSAN group).
Sources:
Read also :
- Infographic: the figures for tuberculosis, a disease that is still relevant
- Tuberculosis: it will kill 75 million people by 2050
- Ingrid Chauvin suffering from pneumonia: is it serious?