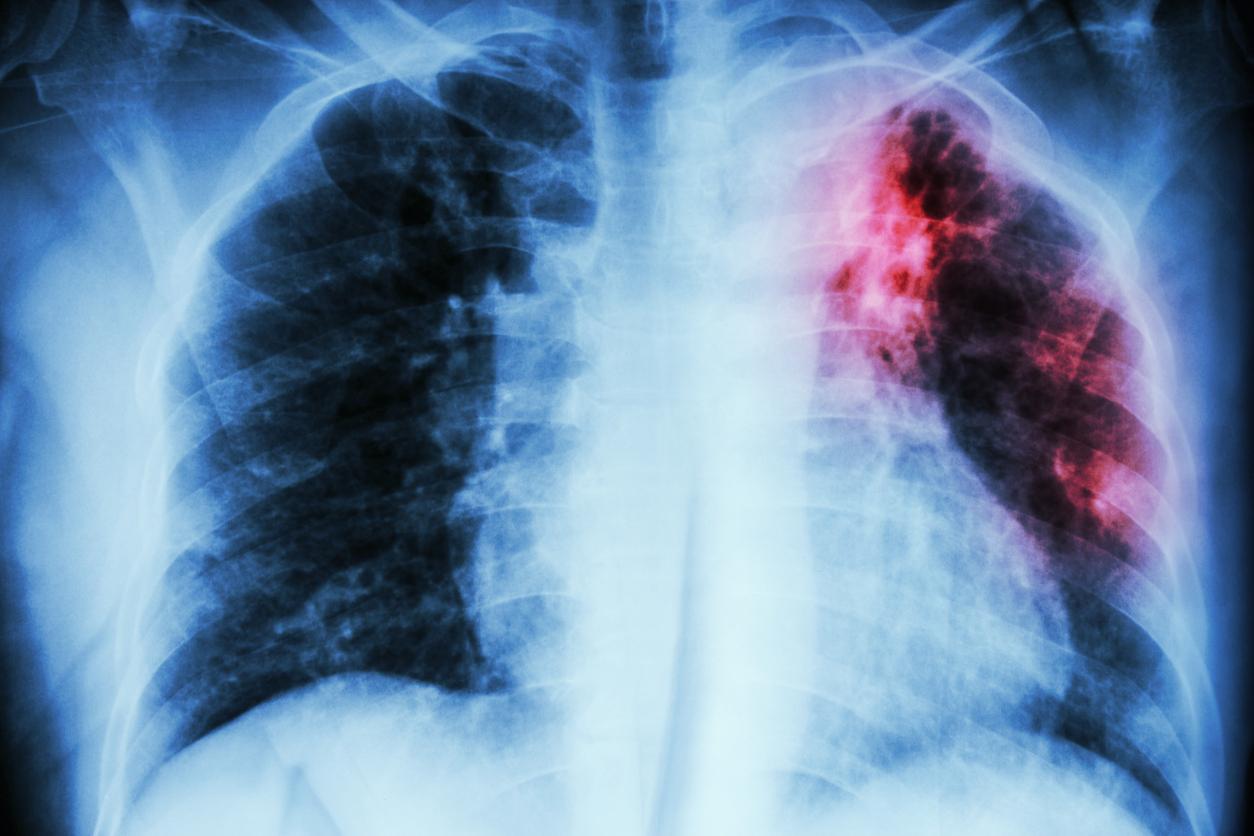
France has 4,700 cases of tuberculosis per year, among which a growing number are resistant to first-line anti-tuberculosis drugs.

Tuberculosis is a rare disease in France. In 2015, just over 4,700 cases were reported. The decline in the number of diagnoses continues. Good news somewhat tempered by the emergence of strains resistant to anti-tuberculosis treatments. The phenomenon is such that it jeopardizes the goal of eradicating the disease by 2035, set by the World Health Organization.
This gloomy observation is made by Professor Jérôme Robert, researcher at the National Reference Center for Mycobacteria and Mycobacteria Resistance to Antituberculosis (CNR-MyRMA). In the latest Weekly Epidemiological Bulletin (BEH), he takes stock of resistance in 2015. It remains infrequent but the trend is worrying. Worldwide, half a million multidrug resistant forms are detected each year.
A poorer prognosis
The study conducted by Prof. Robert looks at 1,472 cases of tuberculosis diagnosed in 2015. Among those never treated, 9% carried a strain capable of withstanding at least one first-line treatment, and 3% had ‘a multi-resistant strain.
The tough mycobacteria are much more present in people who have already consulted for tuberculosis: 18% harbor a multi-resistant strain – therefore capable of surviving isoniazid and rifampicin.
“Resistance to one of the two major anti-tuberculosis drugs has a negative impact on the outcome of the patient and tuberculosis with bacilli resistant to rifampicin have a poorer prognosis than tuberculosis with sensitive bacilli”, explains Professor Jérôme Robert, contacted by Why actor.

80 resistant cases per year
The profile of the patients carrying a resistant mycobacterium is hardly surprising: they are mainly men, originating in 9 cases out of 10 from a country other than France. However, “a good part of the increase in resistance is explained by the fact that a greater proportion of tuberculosis patients diagnosed in France come from countries where resistance is more important, such as the countries of the East”, develops Prof. Robert.
As resistant forms of tuberculosis are on the rise, there is no doubt about it. Until 2011, 30 to 80 multidrug resistant cases were reported each year. Now, 80 is the lower range of cases that are reported to health authorities. The main cause of this phenomenon? Poor follow-up of the treatment that would get rid of the mycobacteria. “The treatment is long, six months for tuberculosis with sensitive bacilli, and contains several antibiotics,” recalls Professor Robert. Stopping it too early therefore favors the selection of resistant mutated strains.
One pill instead of four
But to accuse only the patients would be excessive. “In some countries of the South, the poor quality of drugs on the market comes into play”, continues Jérôme Robert. Non-compliance with expiry dates or storage conditions, but also production quality are all problems facing disadvantaged countries.
Once this resistance has developed, its transmission is relatively simple. Tuberculosis is extremely contagious. “A contact person can then develop tuberculosis with an immediately resistant bacillus, without ever having received antibiotics before,” explains Professor Robert. The more resistant bacilli there are, the more transmission there will be. “
However, breaking the vicious circle is not impossible. This requires a flawless health system, capable of rapidly detecting and isolating contagious cases and offering appropriate treatment. According to Jérôme Robert, the CNRs play a major role but the therapeutic offer must also evolve. He thus proposes to bring together “all the antibiotics in the same pill. The patient cannot stop just one and therefore no risk of error which favors resistance when only one of the 3 or 4 antibiotics is taken, ”summarizes the researcher.
.