Overconsumption of antibiotics from a certain age would be associated with a higher risk of inflammatory bowel disease, such as Crohn’s disease.
- This study is observational: it does not establish a causal link, only a correlation.
- Worldwide, approximately seven million people are affected by inflammatory bowel disease.
The abuse of antibiotics is harmful to public health. When overused or misused, these drugs contribute to antibiotic resistance, the resistance of bacteria to treatment. This phenomenon is oneof the most serious threats to global health“, according to’World Health Organization. But the overuse of antibiotics is also a danger to individual health. According to a study published in the specialist journal gutfrequent use of antibiotics increases the risk of inflammatory bowel disease (IBD) in adults.
Antibiotics: understanding their impact on intestinal diseases
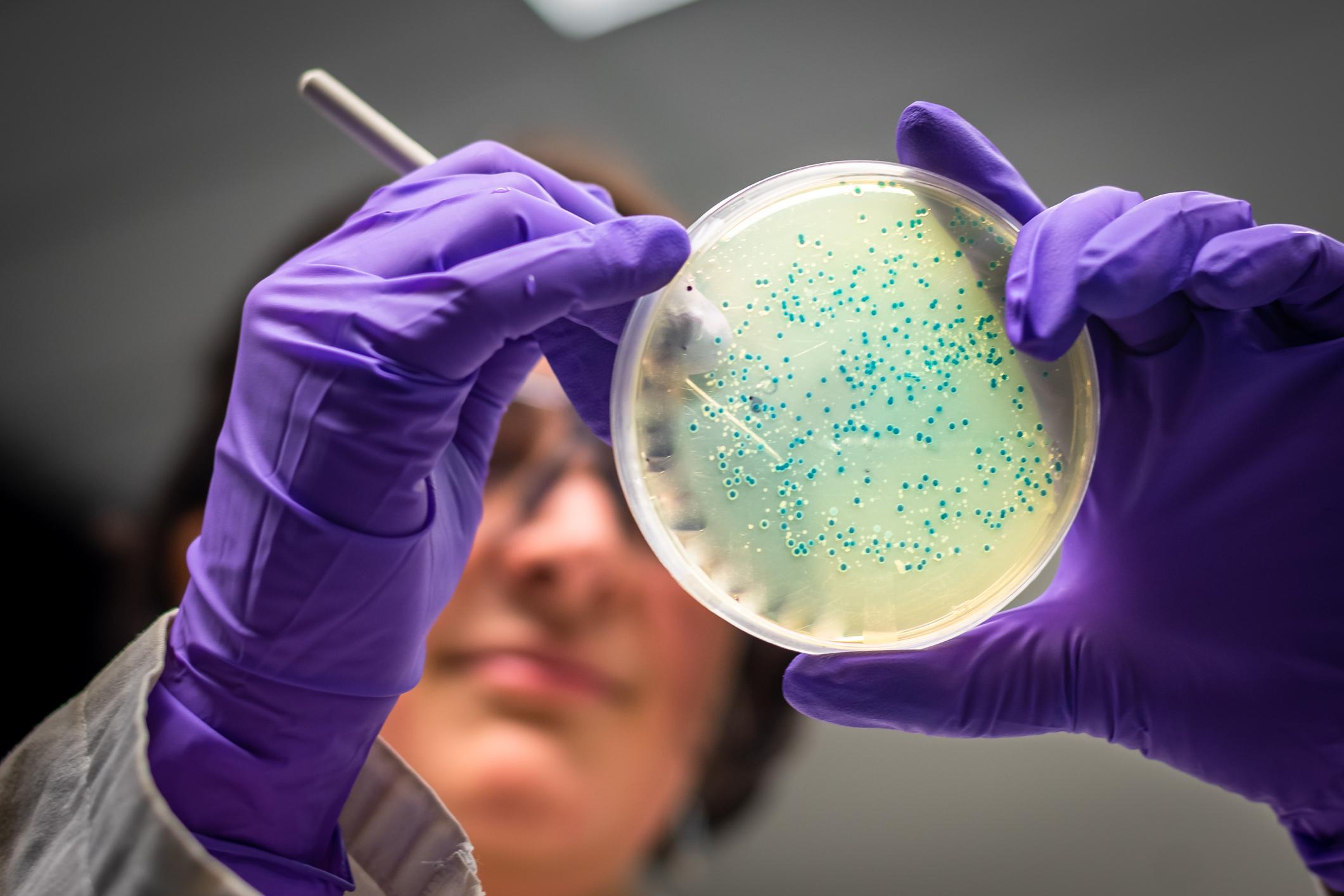
Previous research has shown that antibiotic use may be a risk factor for IBD in young children. But what about adults? To find out, American and Danish researchers used a Danish database: it brought together the medical information of nearly six million people over the age of 10, followed between 2000 and 2018. In total, 91% of participants were prescribed at least one course of antibiotics between 2000 and 2018. During this period, around 36,000 new cases of ulcerative colitis and around 16,900 cases of Crohn’s disease were diagnosed.
Age impacts risk of antibiotic-related bowel disease
Scientists found that antibiotic use was associated with a higher risk of developing inflammatory bowel disease, regardless of age. But the older the person, the higher the risk. People aged 10 to 40 were 28% more at risk of suffering from this type of pathology, compared to 48% for those aged 40-60 and 47% for those over 60.
The authors also noted that the risk was cumulative: each new antibiotic treatment further increased the risk of IBD. “The highest risk of all was seen in people who received five or more courses of antibiotics: 69% increased risk for 10-40 year olds, a doubling of risk for 40-60 year olds, and a 95% increased risk for those over 60″, they note. The negative effects are particularly significant between one and two years after treatment, then they decrease over time.
Intestinal diseases: the most harmful antibiotics
As for the type of antibiotic, nitroimidazoles and fluoroquinolones, which are usually used to treat bowel infections, were the drugs associated with the highest risk of bowel disease. “These are known as broad-spectrum antibiotics because they indiscriminately target all microbes, not just those that cause disease.”say the authors.
How to explain the link between antibiotics and intestinal disease?
According to them, these results confirm a widely held idea: changes in the intestinal microbiome can play a key role in the onset of intestinal diseases. However, many antibiotics have the potential to modify the composition of microbes in the intestine.
They point out that aging is associated with a decrease in the resilience and variety of intestinal microbes and that antibiotics can then aggravate this phenomenon. “Moreover, with treatments by repeated antibiotics, these changes may become more pronounced, ultimately limiting gut microbiota recovery“, they add. The researchers believe that limiting antibiotic prescriptions could reduce the risk of intestinal disease in certain populations, and slow the resistance of bacteria to these drugs.