Following very rare reported cases of immunoallergic thrombosis with dramatic evolution following the administration of AstraZeneca’s anti-Covid vaccine, 2 studies provide a better understanding of how this phenomenon occurs, to prevent or treat it… in order to to continue vaccination.
- The cases of thrombosis following the AstraZeneca vaccine are 1 in 1,000,000, i.e. very rare
- These thromboses occur in association with a drop in platelets
- An association between the Spike protein contained in the vaccine and endothelial cells could be the cause
- Treatment with non-heparinic anticoagulants and high-dose intravenous immunoglobins would be effective.
The New England Journal of Medicine publishes 2 small series of thrombocytopenia with disseminated intravascular coagulation and multiple thromboses after AstraZeneca vaccination. These thromboses include thromboses of the upper sagittal cerebral venous sinus, with fatal evolution, and occurring 5 to 16 days after a first injection of the Covid-19 AstraZeneca vaccine. MoonNorwegian, concerns 5 healthcare professionals and the other 11 people in Germany and Austria.
The average age of those affected, mainly women, is 36 years old (22 to 49 years old). The cause would be secondary to the appearance of an auto-antibody of the “Heparin-Induced Thrombocytopenia” type, systematically found, and which would be capable of triggering coagulation. According to the authors, treatment with non-heparinic anticoagulants and high-dose intravenous immunoglobulins, administered early enough, would be effective.
Alert without frightening
The thrombologists were very surprised by the profile of the patients who had these atypical thromboses since they were mostly women, young, with very unusual site thromboses, for example at the abdominal level, on large vessels such as thromboses portals, and cerebral venous thrombosis, which is very rare.
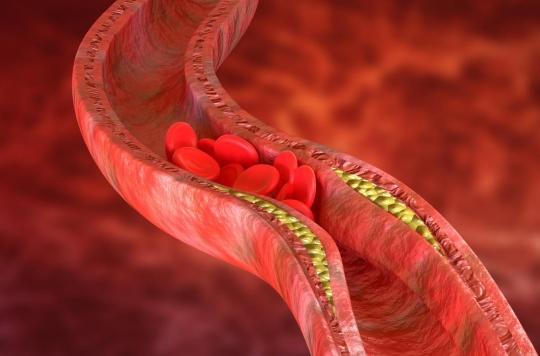
Above all, these thromboses occurred in association with a drop in platelets, exactly as in a “consumption coagulopathy”, a generalized activation of blood coagulation. So basically something catastrophic in young women who had just received the AstraZeneca vaccine.
But we must also be right because these cerebral thromboses are exceptional: if the incidence of thromboses in France is around 1 in 1000, for cerebral thromboses we are at less than 1 in 100,000. With the vaccine, we is on an incidence of about forty cases of atypical thrombosis out of 30 to 40 million people vaccinated in Europe, that is to say close to 1 in 1 million.
So these are particularly rare thrombotic accidents, which also exist with other adenovirus vaccines and from which mRNA vaccines are probably not exempt.
Why atypical thrombosis?
The question arose of why these atypical thrombosis occurring as a disproportionate inflammatory reaction.
The clinical picture of moderate to severe thrombocytopenia and thrombotic complications at unusual sites, beginning approximately 1-2 weeks after SARS-CoV-2 vaccination with AstraZeneca, suggests a disorder that clinically resembles severe thrombocytopenia induced by SARS-CoV-2. heparin, a well-known disorder caused by platelet-activating antibodies that recognize multimolecular complexes between cationic PF4 and anionic heparin.
In recent years, it has been recognized that triggers other than heparin can cause a prothrombotic disorder that strongly resembles heparin-induced thrombocytopenia, both clinically and serologically, including certain polyanionic drugs, but not only, and for example after viral and bacterial infections or prosthetic knee surgery. These various clinical scenarios with apparent non-pharmacological triggers have been classified under the term “heparin-induced autoimmune thrombocytopenia”.
explore to understand
This is what led the German team and the Norwegian team to search for auto-antibodies of the HIT type, or “Heparin-Induced Thrombocytopenia”, that is to say that these patients developed autoantibodies. -anti-PF4 antibodies which would resemble what is described in the vascular storms of HIT with a sort of disseminated intravascular stimulation and overactivation of platelets, endothelial cells, monocytes… even though these women had not received heparin .
You should know that we have on the surface of our vessels, on the endothelial cells, what looks like heparin: these are glycosaminoglycans, sugars, which line our endothelial cells and it is possible that the Spike protein, which was therefore received during this vaccination, associated with these glycosaminoglycans in certain circumstances, and mimicked what could serve as an immune trigger signal, with the appearance of autoantibodies, which turned against the patient’s platelets, inducing thus a major hypercoagulability and these particularly dramatic thromboses.
But, in the end, it is a very rare autoimmunity, occurring on a very particular ground, rather feminine and young favorable to autoimmune reactions, with the possibility of immune dysregulation.
Prevent immune aggression
The iatrogenic risk is never zero, including for a vaccine, but everything must be done to reduce it. First, be aware that in some patients, venous or arterial thrombosis may develop in unusual sites such as the brain or abdomen, which becomes clinically apparent approximately 5 to 20 days after vaccination. If such a reaction is accompanied by thrombocytopenia, it may represent an adverse effect of the preceding Covid-19 vaccination.
In this context, Professor Ismaël Elalamy reminds that it is preferable to take care to prick intramuscularly and not intravascularly, and therefore check for the absence of blood return before administering the vaccine.
It is also necessary to check in the aftermath of the vaccine that there is no local ecchymotic or extensive purpuric reaction, very painful, which should alert on a totally disproportionate general reaction which can occur at the general level with an aberrant inflammatory reaction.
Explore to treat in time
In the event of signs, pain, oedema, intense or stubborn headaches, dizziness, visual disturbances, vaccinated persons must consult urgently for a confirmatory clinical examination, a blood count to check the rate of platelets and try to objectify thrombosis by imaging.
According to the authors of these studies, the curative treatment must be implemented without waiting for all the results with a non-heparin anti-thrombotic treatment or direct oral anticoagulant, which does not interfere with the heparin-dependent pathway.
The Germans also propose to administer high doses of intravenous immunoglobulins to inhibit platelet activation. This recommendation parallels emerging experience in the treatment of severe heparin-induced autoimmune thrombocytopenia, in which high-dose intravenous immunoglobulins have resulted in a rapid increase in platelet count and de-escalation of hypercoagulability.
.
















