According to an FHF survey, the use of certain surgical procedures varies from one to two depending on the region. Disparities that raise questions about the relevance of care.

The relevance of care is a long-term battle, waged by the public authorities for several years. Not only does unnecessary care pose undue risks to patients, but it is extremely costly for the health system: between 20% and 30% of the health care budget. according to estimates, necessarily with a ladle. Enough to provide additional motivation, in these times of budget scarcity.
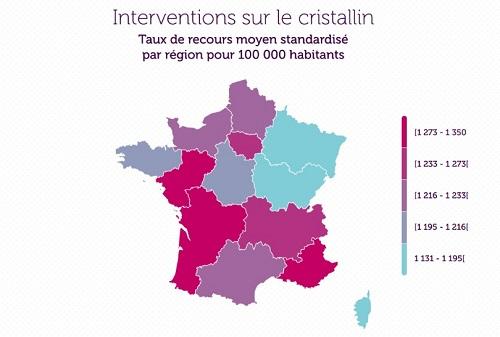
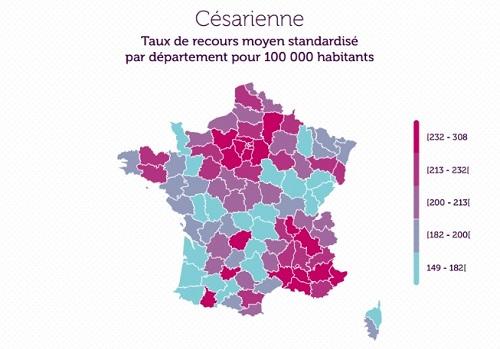
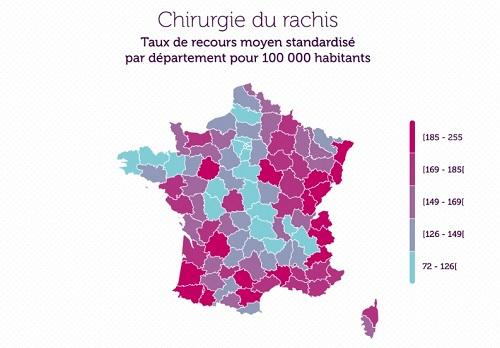
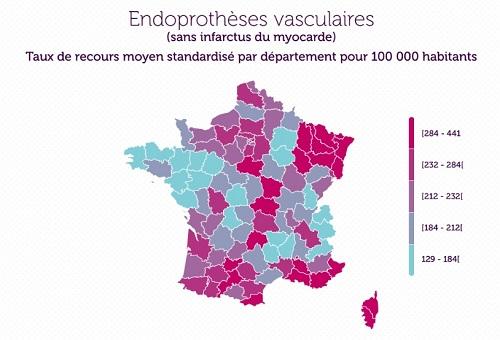
In a survey published on November 26, the Federation of French Hospitals (FHF), the public hospital union, tackled the problem from the perspective of regional disparity. By focusing on four common surgical procedures, reputed to be freely prescribed: cesarean section, lens surgery (cataract operation), spine surgery (sciatica), coronary bypass surgery (angina pectoris or myocardial infarction) and placement of stents (angina pectoris).
By reducing the number of interventions to the population, and controlling for disparities in age and sex, it is possible to compare the greater or lesser liberality with which an intervention is prescribed. And depending on the department, we therefore end up with recourse rates that can vary from single to double!
From single to double depending on the region
You will thus have twice as likely to give birth by cesarean section in PACA or in the Paris region than in New Aquitaine. The reverse is the case for spine surgery: Provencal people have back surgery twice as much as Parisians. And so on … Despite their probable anatomical resemblance, the average Breton receives half as much stents than the Alsatian. Very parsimonious, it also consumes two times less coronary bypass surgery than its neighbor from Normandy. So many disparities that invite us to question the need to improve practices.
In all cases, these are procedures where the risk is well controlled, well reimbursed by health insurance, and for which the temptation is great to prescribe beyond the patient’s needs. This is true for private clinics, generally in a logic of specialization and profit-seeking, but also in public hospitals, that pricing per activity and the reduction in operating budgets also lead to favoring the most remote acts. more profitable, to finance the others. Patients are sometimes also demanding, as is the case with “comfort” cesarean sections.
Hospital financing reform
“The results are final,” concludes the FHF in its press release. “It is urgent to take action and health actors like the French are ready to change their practices,” adds the public hospital union, referring to a second survey showing that the French are in favor of a better control of the appropriateness of care.
If the relevance of care is a long-term work, which relies on the action of supervisors but also of learned societies, a consensus seems to emerge in the world of health. On the occasion of the presidential campaign, the Comité des interassociatif sur la santé (Ciss), the main users’ association, presented a set of measures in this direction. One of the most important, concerning the financing of the hospital, is in the course of preparation, with the introduction of a part of financing centered on the relevance of the care. A question that we have not finished hearing about.
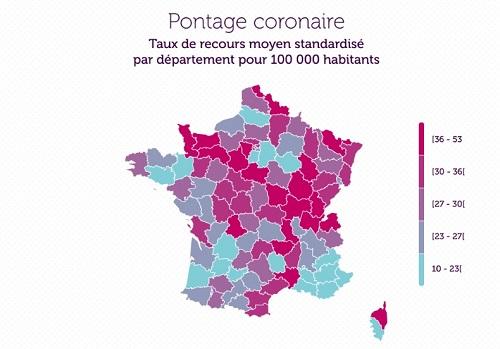
Source: Atlas of variations in practice 2017, FHF.
.

















