Chronic periodontitis, an infection that gradually destroys the gums and causes a loss of teeth, would have a link with Alzheimer’s disease. The presence of the bacteria at the origin of periodontitis was identified in the brain of dementia patients and would have an effect on the production of amyloid plates in question in the appearance of Alzheimer.

- Chronic periodontitis is a disease that reaches gums and can cause teeth.
- Elements of the bacteria that cause periodontitis are present in the brain of patients with Alzheimer’s.
- No causal link between periodontitis and Alzheimer’s, however, was established.
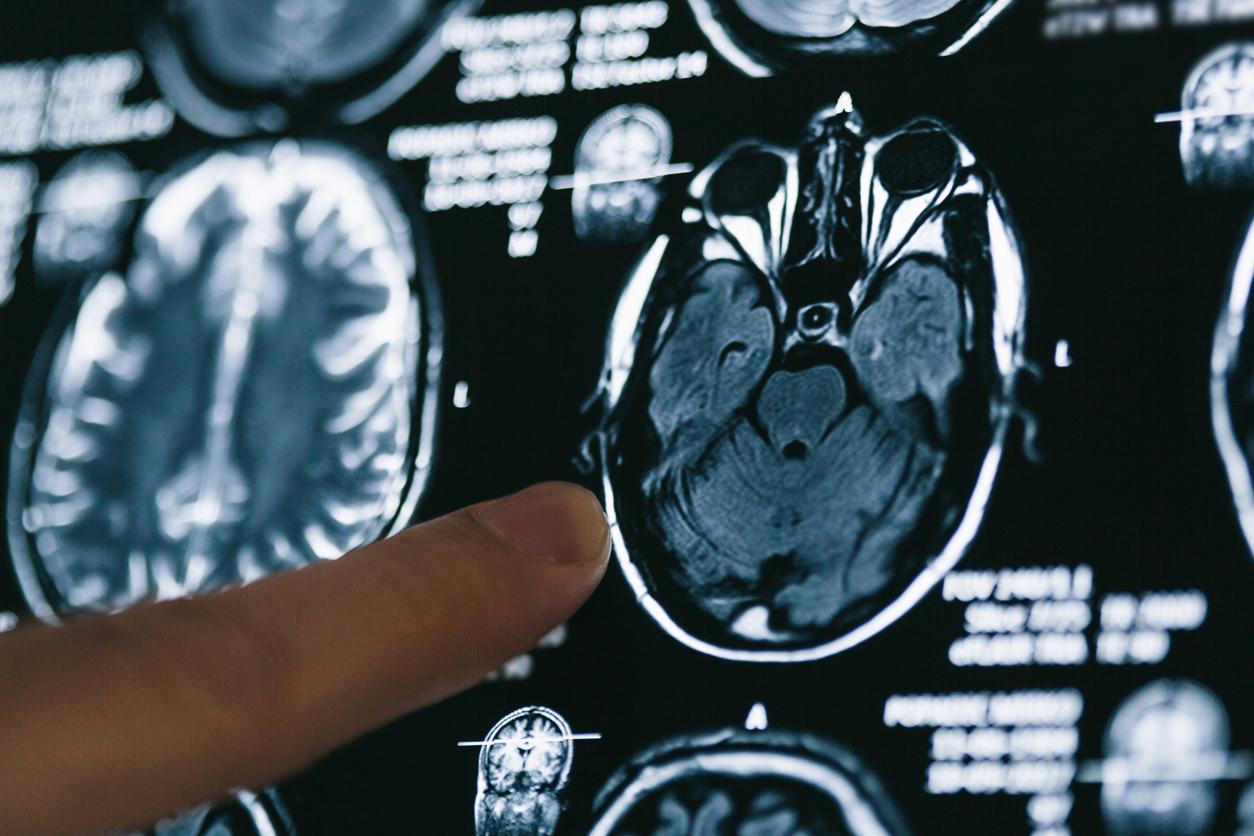
Does the pathogen of chronic periodontitis -Pornomonas gingivalis-would have a link with Alzheimer’s disease? Toxic proteases of this agent, called gingipaïnes, were indeed identified in the brain of patients with this cerebral degeneration.
The track of an infectious cause in Alzheimer’s disease is the subject of numerous works on this form of dementia which today affects more than a million people in France. And a recently published study in Science Advances, which establishes this link between chronic periodontitis and Alzheimer’s, comes to bring a new element in this research axis.
More a risk factor than proven causality
Admittedly, at this stage, the authors of the study evoke more, about this link between chronic periodontitis – an inflammation which gradually destroys the teeth support device – and Alzheimer’s disease, a risk factor than a proven causality. But their work on animal models show that oral infection with gingivalis porphyromonas in mice has led to the colonization of the brain generating an increased production of an amyloid plates, these aggregates which are formed around neurons by preventing them and the neurotransmitters from working well. Even if the role of the accumulation of these amyloid plates in the appearance of Alzheimer’s disease is sometimes called into question, they still remain one of the markers of this form of dementia.
A greater drop in cognition in Alzheimer’s patients with periodontitis
Beyond the experiences carried out in the laboratory and explained in Science Advancesprospective observational studies of patients with Alzheimer’s disease with chronic periodontitis demonstrate a significant drop in cognition over a period of six months compared to Alzheimer’s patients without chronic periodontitis. Hence a certain credit to be given to the hypothesis that the pathogenic agent of this disease could play a role in Alzheimer’s.
The bacteria at the origin of periodontitis could serve as a differential marker in Alzheimer’s
If they do not bring completely convincing elements to the fact that chronic periodontitis could be one of the causes of Alzheimer’s disease, these are looking for a major interest in an evolution in the management of this form of dementia. They show that the inhibition of gingipaïnes, the toxic proteases of the infectious agent of chronic periodontitis has the potential to modify the observations made on Alzheimer’s patients and that the DNA of this infectious agent could serve as a differential diagnostic marker, the correlation being established between Alzheimer’s disease and the load of gingipaïne in the brain.
The periodontitis pathogen present in 25% of healthy people
The study also specifies, with regard to the pathogenic agent of chronic periodontitis, that it can be, without triggering this pathology, present in 25% of healthy people and without oral disease. A presence that can intervene transiently during chewing, a simple brushing of the teeth, the use of dental wire or during interventions in a dentist.