Without intervention, the problem of multidrug-resistant bacterial infections could worsen and overtake the development of new antibiotics.

- In Europe, antibiotic resistance already causes more than 33,000 deaths a year.
- One of the major concerns is that antibiotic resistance is not specific to a single class of bacteria or virus.
- American researchers have identified how a pathogen that thrives in hospitals and clinical settings becomes resistant.
We speak of antibiotic resistance when microorganisms such as viruses or bacteria have acquired the ability to resist antibiotics. According to the World Health Organization (WHO), antibiotic resistance is one of the greatest threats to health, food security and development worldwide, as it becomes increasingly difficult to get rid of it. potentially pathogenic agents. In Europe alone, antibiotic resistance already causes more than 33,000 deaths a year.
Antibiotic resistance is everywhere
A new study, published in the scientific journal mBio, indicates that this phenomenon could become the next health catastrophe and cause nearly 10 million deaths worldwide in 2050. One of the major concerns is that antibiotic resistance is not specific to a single category of bacteria or virus. . Entirely different species of bacteria can transmit resistance genes to each other via plasmids, small DNA molecules in which they store some of their genes outside the chromosome. When two bacterial cells come into contact, they can copy each other’s plasmids, which makes both species resistant to antibiotics.
Pathogens that adapt to antibiotics within 24 hours
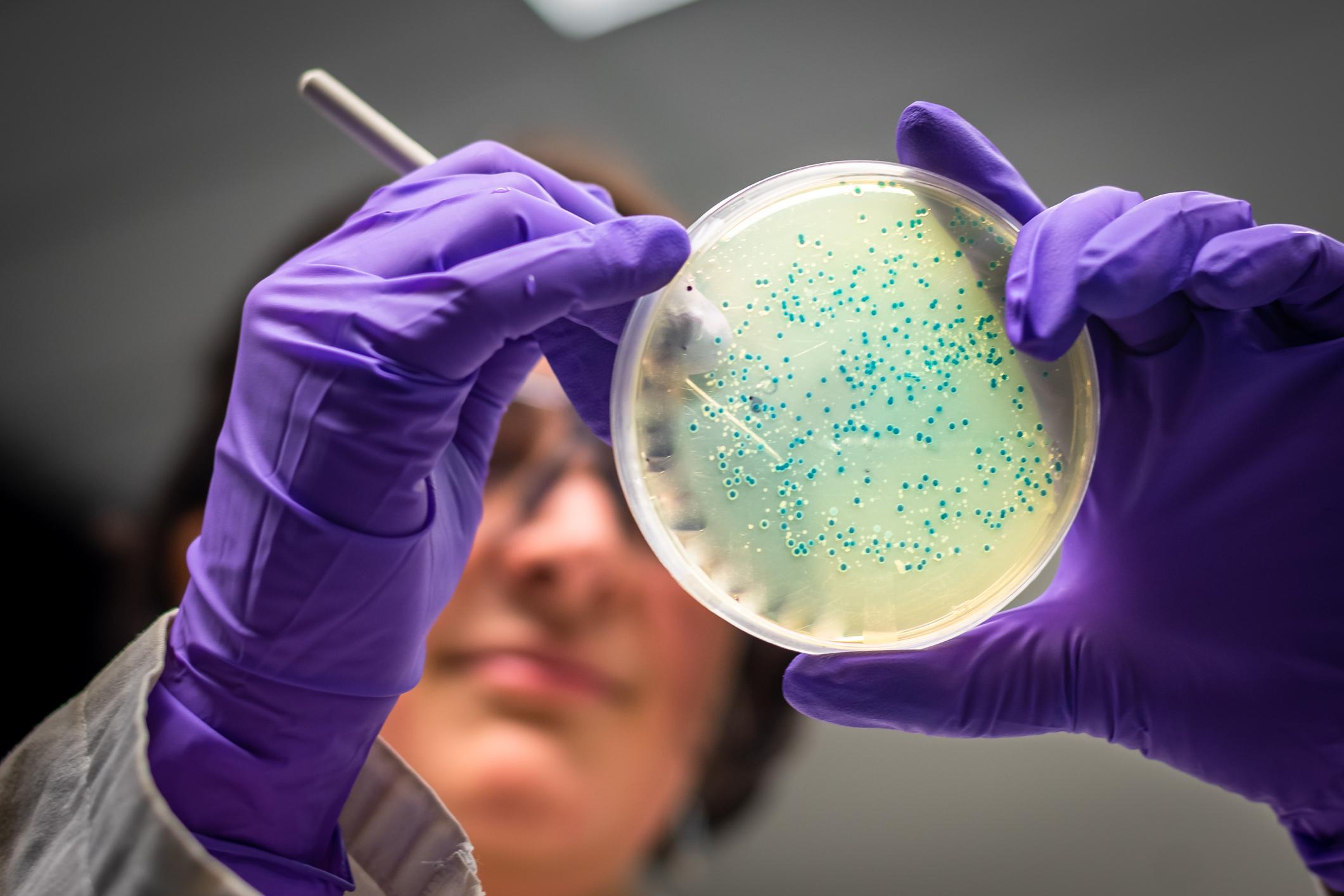
In an attempt to counter this phenomenon and prevent antibiotic resistance from overtaking the development of new antibiotics, American researchers from the University of Texas at Arlington are working to identify and inhibit the defense mechanisms of Acinetobacter baumannii, a pathogen that develops in hospitals and clinical settings. A. baumannii can cause infections in the blood, urinary tract, and lungs, or in wounds in other parts of the body. Infections are usually treated with antibiotics, but many strains are resistant to drugs, including carbapenems, a highly effective class of antibiotics typically reserved for severe multidrug-resistant bacterial infections.
“In previous research, we found that when A. baumannii experiences stress, such as antibiotic treatment, it changes its cell envelope to tolerate the antibiotic for long periods of time.specifies Joseph Boll, author of the study. Specific modifications allow bacteria to survive long enough to develop true antibiotic resistance, which can lead to antibiotic treatment failure. This can happen within 24 hours of exposure to antibiotics.”
Bacterial resistance is progressing irremediably
The researchers identified the adaptations in the cell envelope that allow the pathogen to survive in the presence of antibiotics and how survival contributes to the acquisition of true resistance. They shed light on the role of two enzymes – called LD-transpeptidases – which remodel the cell envelope to promote its survival during antibiotic treatment. Researchers eventually hope to find new cell-surface targets for antibiotics to attack, boosting the potency of existing drugs against A. baumannii infections.
Drug resistant bacteria have prompted healthcare professionals to use therapies where multiple drugs are used to treat bacterial infections. “But even these methods are becoming increasingly ineffective.laments Joseph Boll. It’s become a game. Researchers discover a new antimicrobial, then bacteria become resistant to it. We are out of options. Bacterial resistance is rapidly overtaking the development of new antibiotics.”
.