An important step has just been taken in the development of a new antibiotic based on teixobactin, capable of eradicating numerous resistant bacteria.

Antibiotic resistance is a plague with a great future. Already responsible for 10 million deaths, multidrug-resistant infections point to a major health crisis, for lack of new drugs. This is why the discovery of teixobactin in 2015 had raised enthusiasm. Isolated from the soil microbiota by a team from Northeastern University in Boston, this molecule has the potential to become an essential antibiotic.
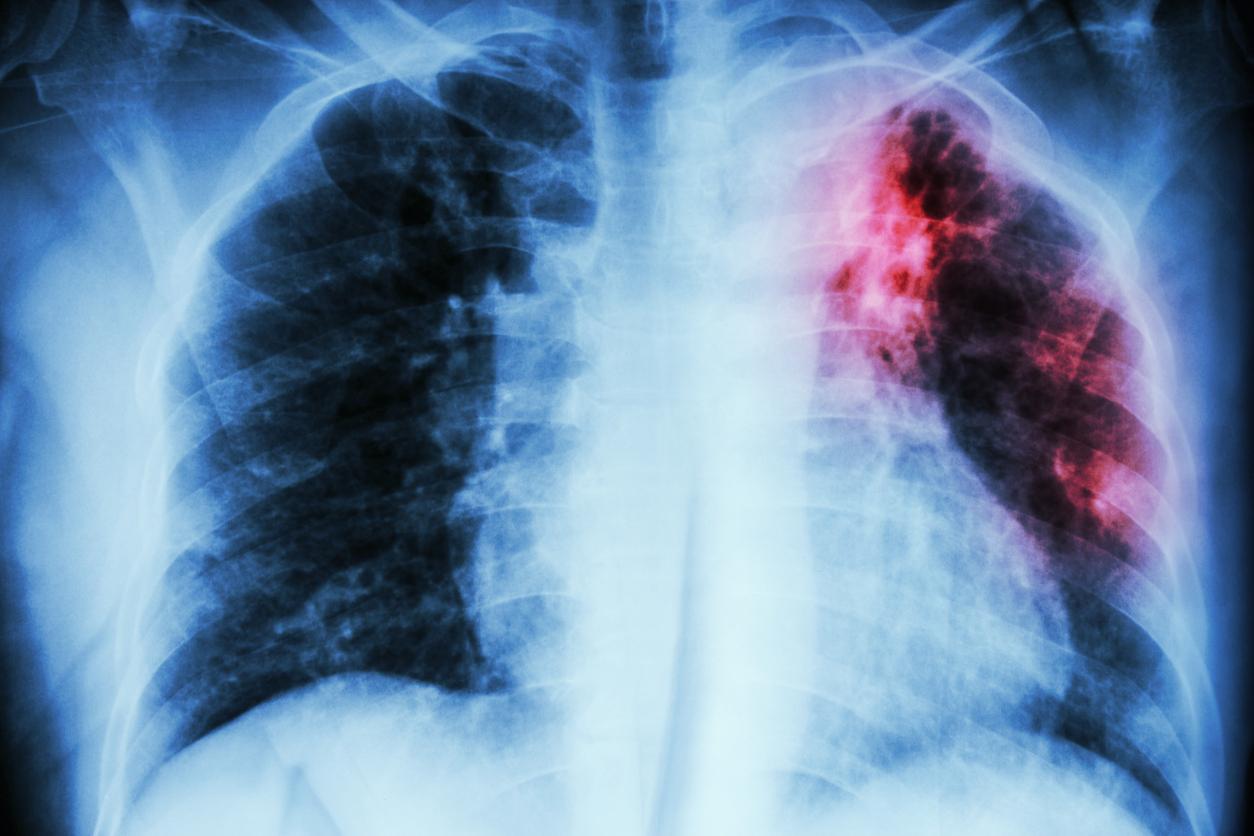
Because teixobactin has the ability to destroy so-called Gram + bacteria by playing on their known resistance mechanisms. Among its proven targets, many celebrities: the tuberculosis bacillus (M. tuberculosis), the bacteria responsible for most pneumonia (S. pneumonia), or even staphylococcus aureus and enterococcus, responsible for serious resistant nosocomial infections.
Active analogues in vivo
But the development of a new drug is a way of the cross. Before arriving at the antibiotic of the future, it is still necessary to know how to produce the molecule on a large scale, in a version that is not toxic to humans. It is in this process that an important step has just been taken, as announced by a team of chemists from the University of Lincoln (United Kingdom) in a published article in the Journal of Medicinal Chemistry.
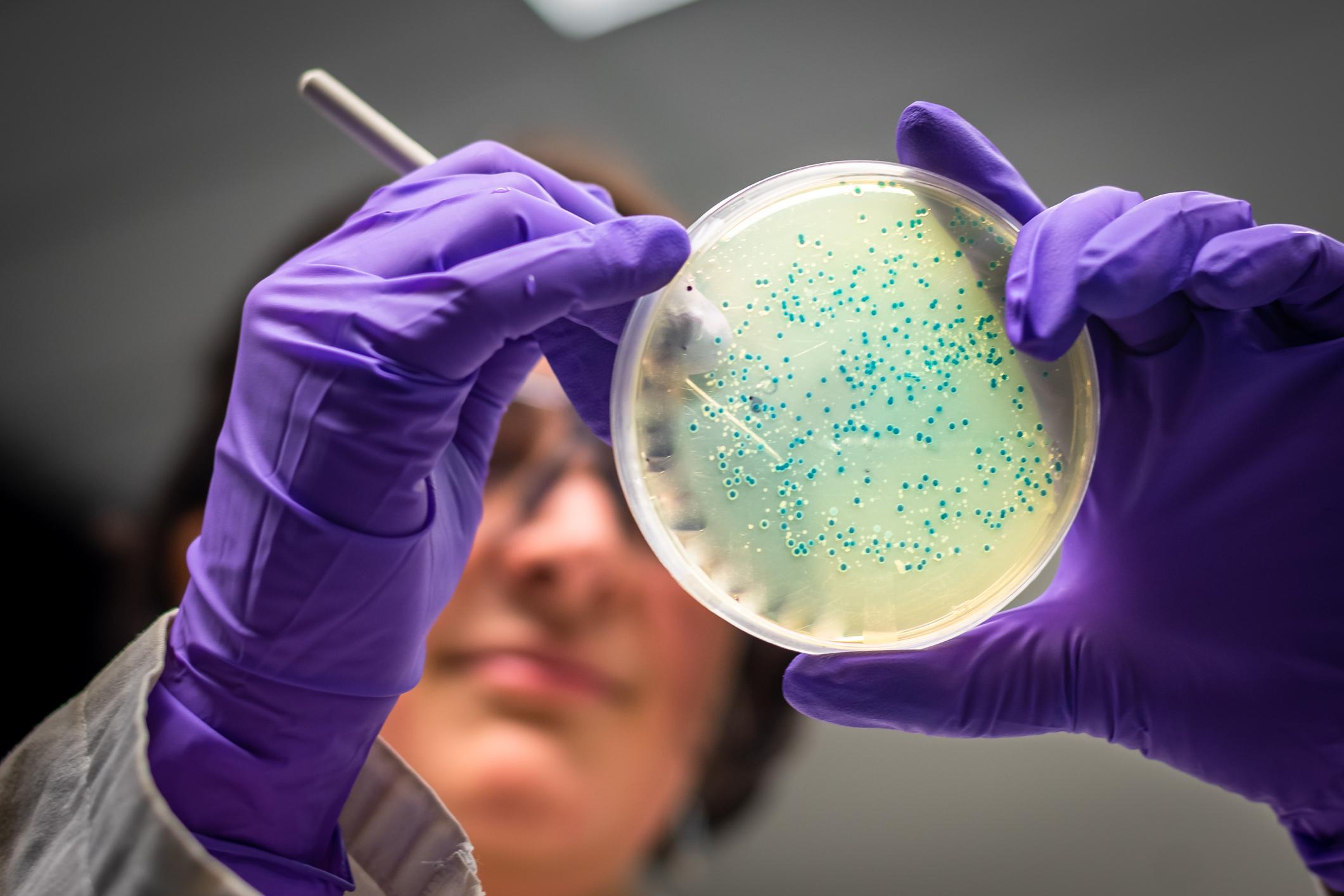
Indeed, the researchers succeeded in producing ten analogues of teixobactin capable of eradicating resistant strains in the laboratory but also in vivo, on mouse corneas. Unlike the original molecule, whose synthesis is as tedious as it is random, these analogues can be made in less than an hour, and appear to be just as active. Valuable tools to hope to achieve the long awaited new antibiotic.
At least six to ten years to wait
“Analogs are fundamental to understanding the therapeutic potential of teixobactins in humans,” says Ishwar Singh, senior author, at Future Science. “There is a high failure rate when trying to transpose a molecule from discovery to clinical use, especially because of secondary toxicities in humans. “
Teixobactin prevents pathogenic bacteria from synthesizing the molecules (peptidoglycans) that make up their outer wall, causing their destruction. At present, no resistance mechanism has been identified. It seems that the molecule attacks fairly fundamental mechanisms that are unlikely to mutate. But biologists remain cautious, because it often takes decades of intensive use for new resistance to appear.
“There is still a lot of work to do before we can end up using teixobactin as an antibiotic in humans”, concludes the chemist. “It will probably be six to ten years before we have a drug that doctors can prescribe to their patients, but it’s a big step in the right direction. “
.