There sickle cell disease is the most common genetic disease in France. It affects the hemoglobin of red blood cells and manifests itself in particular by anemia, painful crises and an increased risk of infections. While current treatments have greatly increased the life expectancy of affected patients, they are still limited and the consequences of sickle cell disease can be serious.
The manifestations of sickle cell disease can appear from the age of 3 months and have very serious repercussions for the health of the child. Sickle cell disease is, for example, the leading cause of childhood stroke. Without early treatment, the infant mortality rate in children with sickle cell disease is very high. In children under 5 with this disease, the first cause of death is the occurrence of infections. Early detection of the disease can enable preventive measures to be put in place (anti-pneumococcal vaccination, preventive treatment against invasive pneumococcal infections).
Hence the importance of detect babies as soon as possible.
Currently, in France, its screening is recommended at birth but it is not systematic for newborns. It is carried out in a targeted manner, only for babies whose parents have origins at risk (for example: West Indies, Guyana, Reunion, sub-Saharan Africa, Brazil , Madagascar, Mauritius, Algeria, Tunisia, Morocco, Southern Europe….).
At the request of the General Directorate of Health, HAS looked into the question of broader screening. After studying recent epidemiological data, it recommends this November 15 (see review) that screening for sickle cell disease is extended to all newborns.
Why screen all babies at birth?
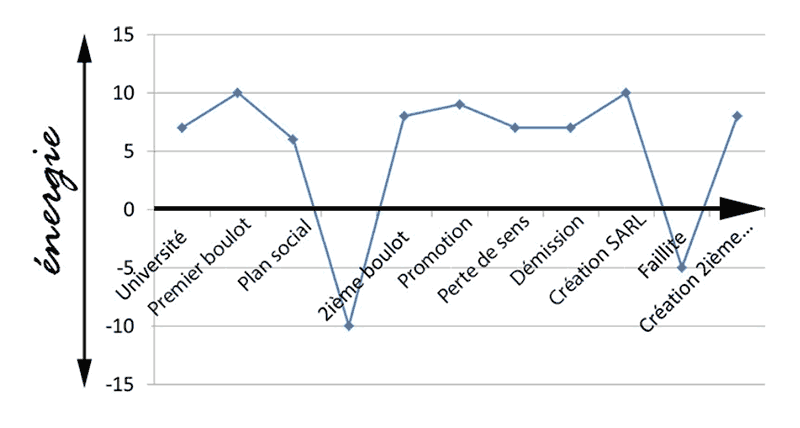
HAS justifies this opinion by the increase in the incidence of sickle cell disease since 2010. Thus, it is the only disease screened at birth whose incidence is increasing regularly: 557 cases were screened in 2020 compared to 412 in 2010.
Another argument for systematizing screening: unequal access from one region to another. Thus, more than three out of four children benefit from it in Ile-de-France, against barely one in two nationally in 2020, while no region in France is unscathed. of cases.
Finally, according to the HAS, some newborns yet in the target did not benefit from screening, hence a high loss of chance for the children.
A powerful test
HAS recalls that the screening test used is very effective, in particular, no false positives have been reported in 20 years. It is carried out on the same medium (Guthrie test) as the other screening tests carried out at birth.
All of these reasons lead the HAS to recommend stopping targeting in favor of neonatal screening for sickle cell disease extended to all newborns.
The Ministry of Health should validate this opinion quickly. In practice, remember that neonatal screening is free: it is most often carried out at the maternity ward, between 48 and 72 hours after birth. Parental consent is required.
It takes the form of a mini “blood test” carried out by taking drops of blood on a blotter, after a small prick in the newborn’s heel. The results are analyzed quickly and, if a pathology is detected, treatment is immediate. See also the other diseases screened at birth.