First reason for consultation with the general practitioner and in the emergency services, pain affects more than one in five French people. In question, often acute pain that occurs during an accident or illness. This unpleasant sensation then acts as an alarm signal. Sometimes, however, pain appears without it being possible to identify a precise origin (fibromyalgia for example) or/and settles down over time, resists treatment, and leaves less and less respite to those who suffer from it.
Physical or psychological pain: many analogies
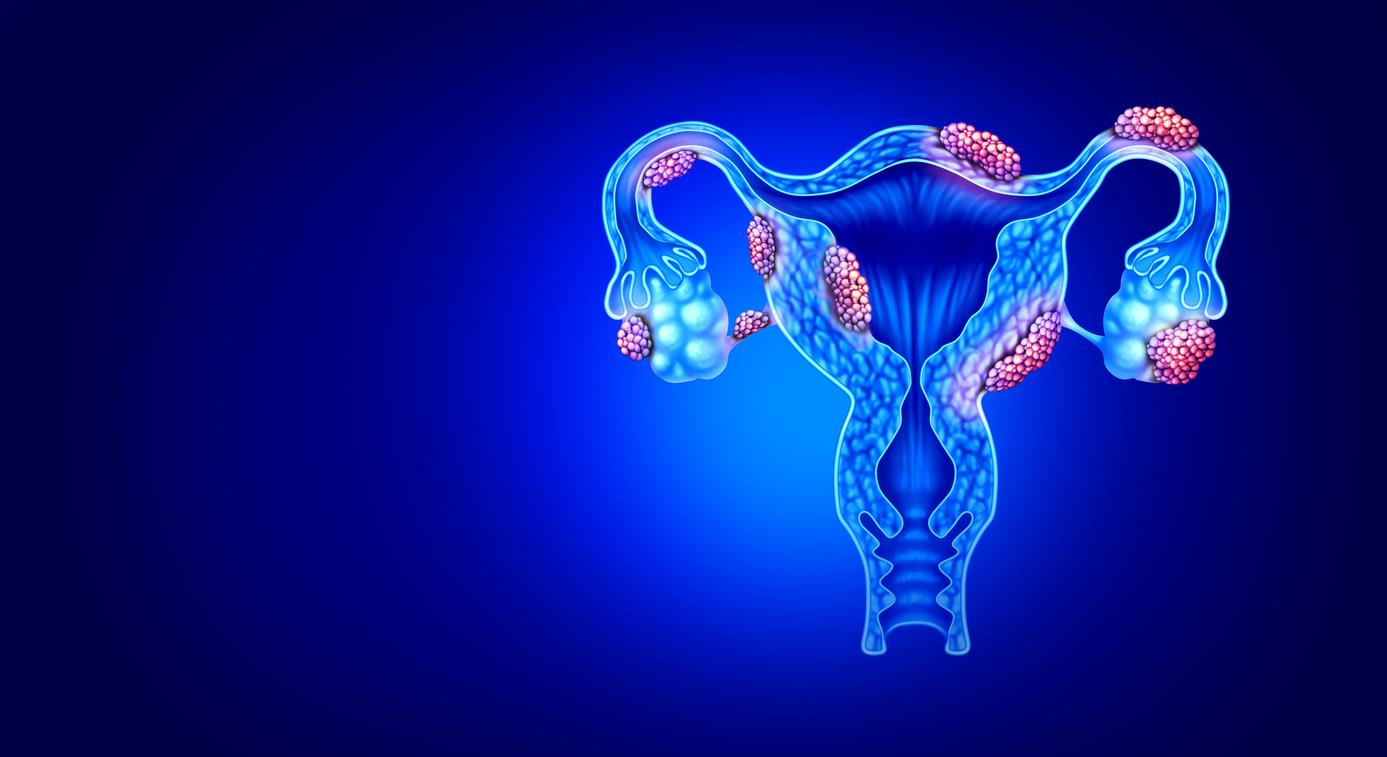
We perceive this exacerbated sensory reaction with specialized nerve endings (2000 to 3000 nociceptors per mm2) located under the skin, in our viscera, around the muscles, at the level of the heart… The nerves then conduct the painful messages to the spinal cord , which itself transmits them to the brain allowing us to “feel” it and memorize it.
Neurobiologist Michel Lazdunski notices many analogies between physical pain, which can become chronic, and psychological pain, which frequently leads to depression and/or post-traumatic stress. Pain is perceived subjectively, according to our sensitivity, our personal history, our culture, our relationship to illness, etc.
Pain is a challenge for the doctor
pain hypersensitivity could be related to psychological factors, such as “certain personality traits, difficulty in identifying and expressing emotions, or even a traumatic experience associated, for example, with mistreatment or sexual abuse”, notes Dr. Didier Bouhassira, neurologist. Therefore, the treatment that works for one may not provide relief for another. That’s the whole difficulty.
Moreover, according to the French Society for the Study and Treatment of Pain (SFETD), 70% of people who suffer from moderate to severe chronic pain do not receive appropriate treatment. “Pain is a challenge for the doctor, he must know how to adapt admits Dr. Patrick Sichère, rheumatologist.
In order not to let it set in, before surgery for example, doctors are increasingly taking into account the risk factors for chronic pain (anxiety, depression, gender, etc.), in order to optimize and individualize care.
>> And when the pain is already there? “IYou have to start by listening and reassuring the patient. Then, offer him multidisciplinary care, combining medication, therapeutic education, rehabilitation, psychological help and as many techniques that will help relieve him and allow him to regain control over the pain.