Despite all disinfection precautions, antibiotic-resistant bacteria remain on hospital floors. It is possible to find traces of it in a completely sanitized room, less than 24 hours after disinfection.
-1604055688.jpg)
- Some bacteria resistant to antibiotics would be able to develop in hospitals.
- Carried by the shoes of caregivers, these bacteria would take less than 24 hours to colonize a sanitized room.
Despite repeated disinfection, hospital floors are breeding grounds for bacteria. This is the conclusion of the work carried out for the Decennial 2020, the sixth international conference on health care, which was canceled due to the Covid-19 pandemic. The conclusions, which were nevertheless published in the supplement of the journal Infection Control & Hospital Epidemiologyreturn to the resistance of bacteria to antibiotics, which survive on floors and in hospital rooms.
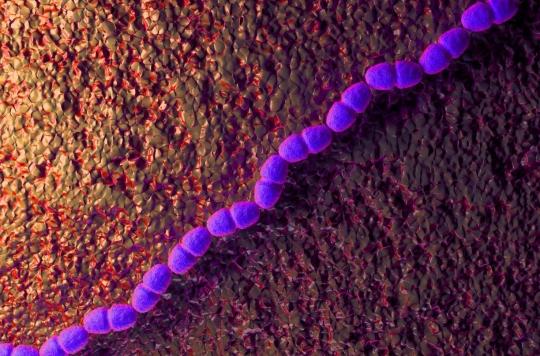
Staphylococcus aureus and enterococci
“If the bacteria remained on the floors it wouldn’t matter, but we are seeing clear evidence that these organisms are being transferred to patients, despite our current control efforts., says Curtis Donskey, lead author of the study and epidemiologist at Cleveland Hospital (USA). L’Hand hygiene is essential, but we need to develop practical approaches to reduce underappreciated sources of pathogens to protect patients.”
With colleagues from the Louis Strokes Medical Center, he was able to follow the contamination of 17 new patients admitted to hospital rooms. The goal was to identify when and how bacteria entered patient rooms. For this, the rooms were meticulously cleaned and disinfected, and all patients tested negative for methicillin-resistant staphylococcus aureus (MRSA) as well as other bacteria likely to be observed in this environment.
The researchers then analyzed the interactions between caregivers and patients, as well as portable medical equipment that can be moved from one room to another. Three times a day, samples were taken from the patients, their socks, their beds, the floor and other frequently used surfaces.
Rapid infection
Within the first 24 hours, half of the rooms tested positive for Staphylococcus aureus. Four days later, 58% of rooms were also infected with vancomycin-resistant enterococci (VRE). Most often, bacterial contamination started on the floor, then moved onto patients’ socks, onto their bedding and onto other surfaces.
“Although our research demonstrates that these bacteria can find their way into and around a patient’s room, not everyone who encounters a pathogen will become infected.however, reassures Sarah Redmond, lead author of the study and a student at Case Western Reserve University School of Medicine. But with that in mind, are there simple ways to treat these exposure areas?”
In another study published last August in Iinfection Control & Hospital Epidemiologythe researchers were already pointing to this same situation concerning SARS-CoV-2, which was found on the floors and shoes of health personnel in Covid units.
However, further research is still needed to elucidate the role of soil contamination in the transmission of pathogens, both bacterial and viral. The researchers themselves also remain critical of the limits of their own study, in particular with regard to the size of the sample, and other variables which would not have been taken into account at the level of the health personnel, this which may prevent generalization of the results to other hospitals.
















-1609908030.jpg)