Targeted therapies and anti-cancer immunotherapies, which are not very effective against primary prostate cancers, could perhaps work against bone metastases.

the Prostate cancer is the most diagnosed in men worldwide. It is estimated that approximately one in seven men will be affected in their lifetime. Diagnosed early, this cancer is very treatable and many patients never even need treatment, their affliction being monitored from afar. So much so that the survival rate for men with localized prostate tumors detected early is almost 100%. However, sometimes the disease is diagnosed too late and the cancer has spread to the bones. In which case, it becomes severe and incurable: the five-year survival rate is only 29% for men with prostate bone metastasis. New work could, however, help to better overcome this form of disease.
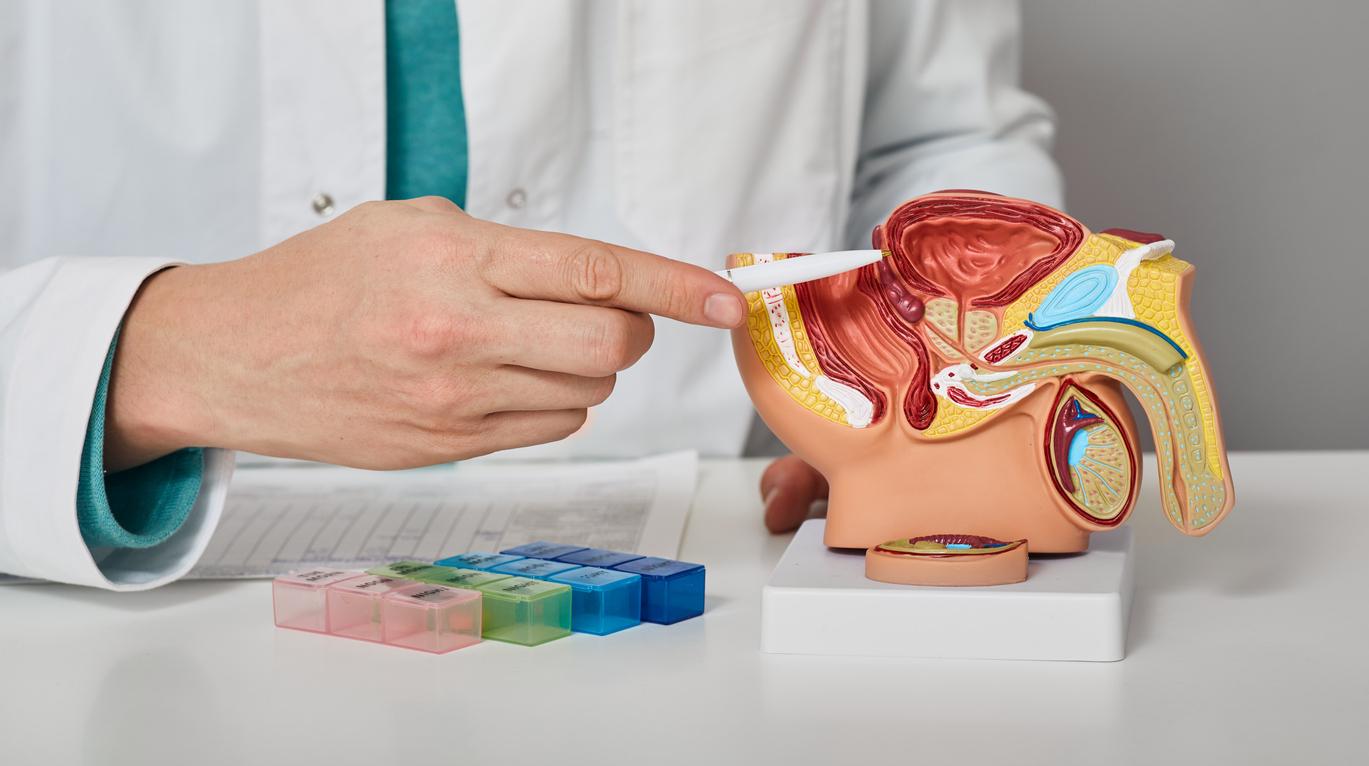
Currently, lytic metastases, which destroy bone tissue, and blast metastases, which build new bone tissue from cancerous cells, are treated the same as the primary prostate cancers from which they arise. . However, according to a study published in the Journal for Immunotherapy of Cancer, this way of proceeding would be wrong. According to researchers from the Cancer Center at the University of Colorado (United States), targeted therapies and cancer immunotherapies, which are not very effective against primary prostate cancers, could perhaps work against bone metastases, together or separately depending on their nature. Targeted therapies are a fairly new type of treatment, which more specifically attacks cancer cells by targeting cancer-specific abnormalities, while less disrupting normal cells, while immunotherapy stimulates the patient’s immune system to strengthen its defenses against cancer cells
“We studied a collection of human bone tissue samples (…), containing prostate cancer and showing characteristics of lytic or blast disease”, explain the researchers. During their work, the latter noticed that the genetic and cellular landscapes of these two types of metastases differed.
Directly measure immunotherapy in bone metastases
“I was really shocked by the increase in pSTAT3 (gene signal pathway) in blast patients. I expected these bone-producing (blastic) lesions to have few or no specific targets. I am happy to have been wrong, because these are the most common lesions in patients with prostate cancer”, explains Claire Ihle, author of the article.
And, while primary prostate cancers tend not to elicit an immune response, they noticed that both blast and lytic metastases had elevated levels of the protein PD-L1. This could mean they are more likely to respond to the class of cancer immunotherapy called checkpoint inhibitors.
“We have developed a test that can directly measure immunotherapy and pathway targets in bone metastases, explains Philip Owens, first author of the article. It’s important because we could potentially use it as a test to determine which of many immunotherapies might be best for an individual patient, one at a time, and really provide personalized therapy. If I had metastatic bone disease, I would like a pathology department to know that the immunotherapy they want to treat me with has a good target level in the tissue they want to treat,” he continues.
New therapies and drug combinations
Researchers are now working to develop therapies in mouse models of lytic and blast bone metastases. If all goes well, this could eventually pave the way for new therapies and drug combinations for those metastases that make prostate cancer a life-threatening disease.
Currently, hormone therapy is the main treatment for metastatic prostate cancer. It can be given with radiation therapy or chemotherapy.
In May, a study published in the Journal of Clinical Oncology Precision Oncology had previously shown that 57% of 3,500 tumor samples from men with advanced prostate cancer had genomic characteristics indicating that the disease could be cured by targeted therapy. “More than half of the patient tumors in this study have features for which there are drug targets. These results provide critical information on how we can design new clinical trials or drugs that will better treat men with advanced prostate cancer.

.