The rules of rules are common and more or less strong, but they can be the sign of endometriosis if they become chronic and disabling. Here is how to distinguish them, according to a gynecology teacher.

- The menstrual pain is common, but when they become chronic and disabling, they can be the sign of endometriosis.
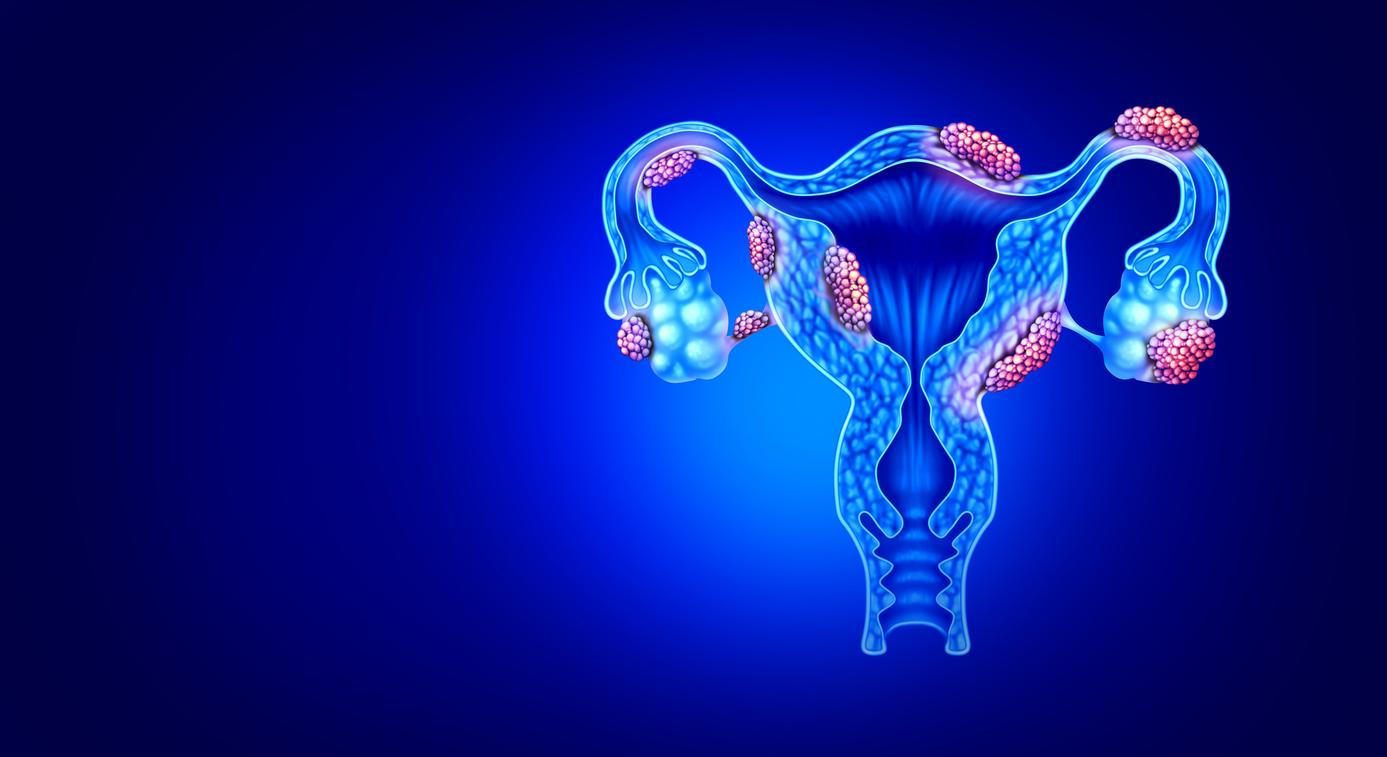
- This disease is characterized by the presence of endometrial tissue outside the uterus, causing pain during rules, sexual intercourse and sometimes digestive and urinary disorders.
- The diagnosis is often based on a laparoscopy, but management must be global: hormonal treatments, physiotherapy and psychological support.
Each month, the rules cause more or less intense pain in many women. But when these pain becomes chronic and disabling, they can be a sign of endometriosis. In an article published in The Conversationthe gynecology teacher Sonia R. Grover, of the University of Melbourne (Australia) explains how to distinguish these two conditions and better ensure their management.
Understanding rules of rules
The rules designate the elimination of the uterine mucosa (the endometrium) which thickens each cycle in anticipation of a pregnancy. When no fertilization takes place, this mucosa stands out and is expelled by uterine contractions, causing more or less strong pain.
The inflammatory substances released during this process also explain the symptoms associated with the rules: nausea, headache, diarrhea, dizziness. In some women, these pains are particularly intense on abundant days of bleeding or during ovulation. About 90 % of adolescent girls feel menstrual pain, and for 20 % of them, these pains are so severe that they disrupt their daily lives.
Endometriosis, persistent and complex pain
Endometriosis is characterized by the presence of fabric similar to the endometrium outside the uterus, often in the pelvic cavity. It can cause intense pain during rules, but also during sex, urinary and intestinal disorders, as well as low back and femoral pain. Certain symptoms such as chronic fatigue or migraines are frequently associated with endometriosis, but can also touch women with pelvic pain without endometriosis.
The diagnosis of endometriosis is mainly based on a laparoscopy, an intervention allowing to observe the pelvic organs. Except that only 50 % of patients with such pain end up receiving a diagnosis of endometriosis. Not to mention, moreover, that certain women with endometriosis feel no pain. “So we cannot predict who has or does not only have endometriosis from symptoms”underlines Sonia R. Grover.
COULD Your Painful Periods Be a Sign of Endometriosis?
Bindi Irwin Experienced 10 years of “insurmountable fatigue, bread & nausea”.
???? These 4 expert articles Help Answer Big Questions about Endometriosis Pain, Diagnosis and Treatment:@westernnsydneyuhttps://t.co/bnvglzqayk
– The Conversation – Australia + New Zealand (@Conversationedu) March 9, 2023

A care that must be global
The management of endometriosis is based on a multidisciplinary approach. Surgery to withdraw lesions is an option, but it is not always final: 30 % of patients find their pain in six months and 50 % undergo a new intervention in the following years.
Hormonal treatments (continuous contraceptive pills, progestin) often relieve pain. But personalization of treatment remains essential because not all patients react in the same way to medication. In addition, global management including physiotherapy, psychological support, adaptation of lifestyle and management of digestive or urinary symptoms is often recommended to improve quality of life.
The fact remains that if your menstrual pain significantly impacts your daily life, do not trivialize them and remember to consult, concludes the researcher. Early diagnosis will allow better management and reduction in suffering.